Medication Smell Risk Checker
Check Your Medication Risk
Dysosmia affects up to 20% of smell disorders and is often missed by doctors. Enter your medication to see if it's linked to smell distortion.
Enter a medication name to see risk level
Common Symptoms
- Metallic taste (like pennies)
- Food tasting like chemicals or garbage
- Phantom smells (smoke, burning)
- Sudden loss of smell
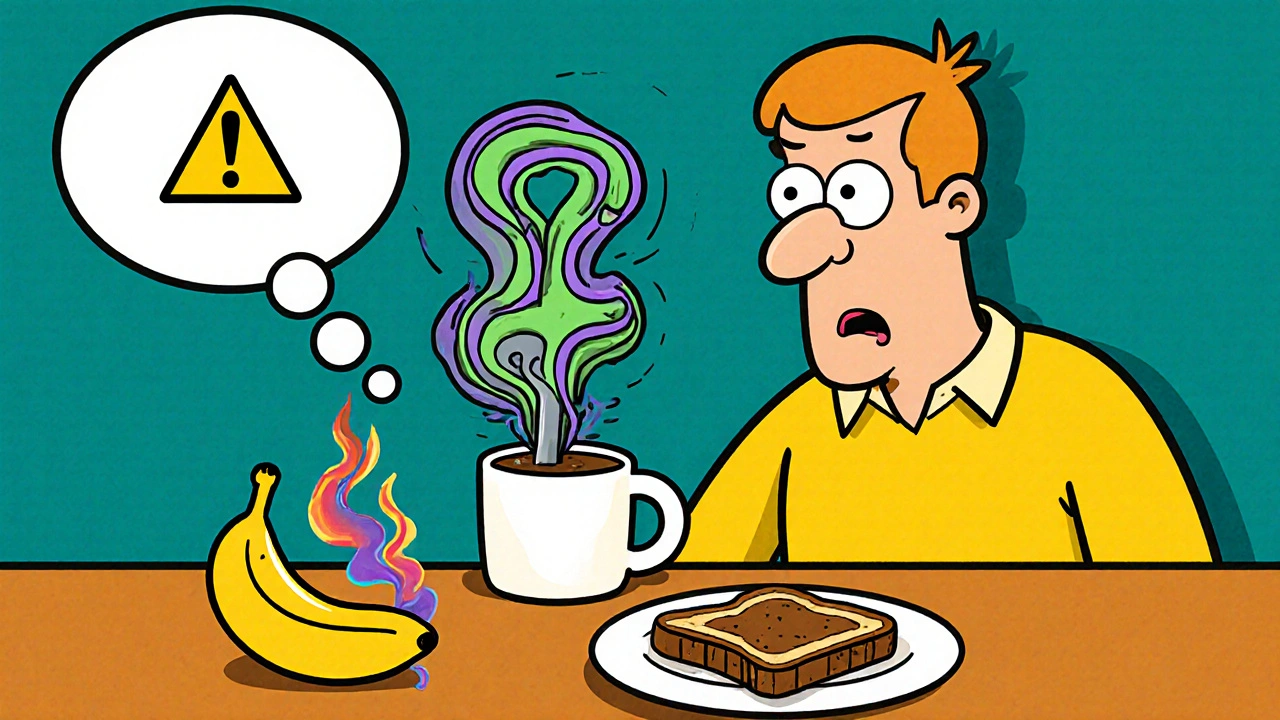
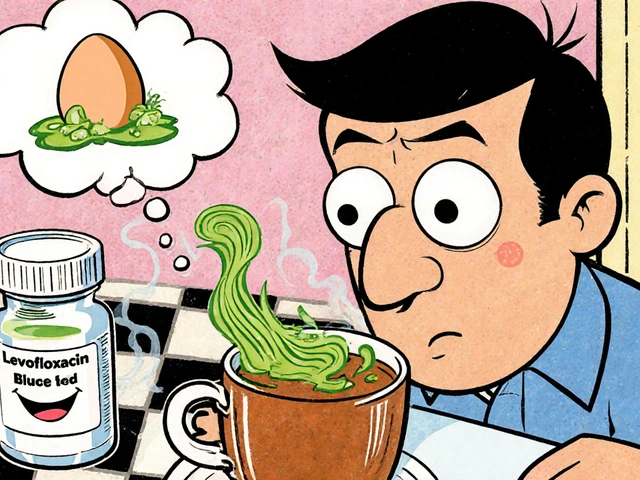
Ever taken a pill and suddenly your coffee tastes like metal, or your favorite food smells like rotten eggs? You’re not imagining it. This isn’t just a weird quirk-it’s a real, documented side effect called dysosmia. It’s when your sense of smell goes wrong. Familiar scents turn sour, bitter, or even disappear entirely. And it’s more common than most doctors realize.
What Exactly Is Dysosmia?
Dysosmia means your brain is misreading smells. It’s not just losing your sense of smell-that’s called anosmia. Dysosmia is when things smell wrong. A banana might smell like gasoline. Bread might smell like burning plastic. Some people even smell smoke or chemicals when nothing’s there. It’s not just unpleasant-it’s disabling.
Up to 20% of all smell and taste disorders come from medications, according to Dr. Richard L. Doty at the University of Pennsylvania. That makes it the second most common cause after colds and sinus infections. And while most people think of antibiotics when they hear about side effects, dozens of other drugs can do this too-blood pressure pills, antidepressants, seizure meds, even some heart medications.
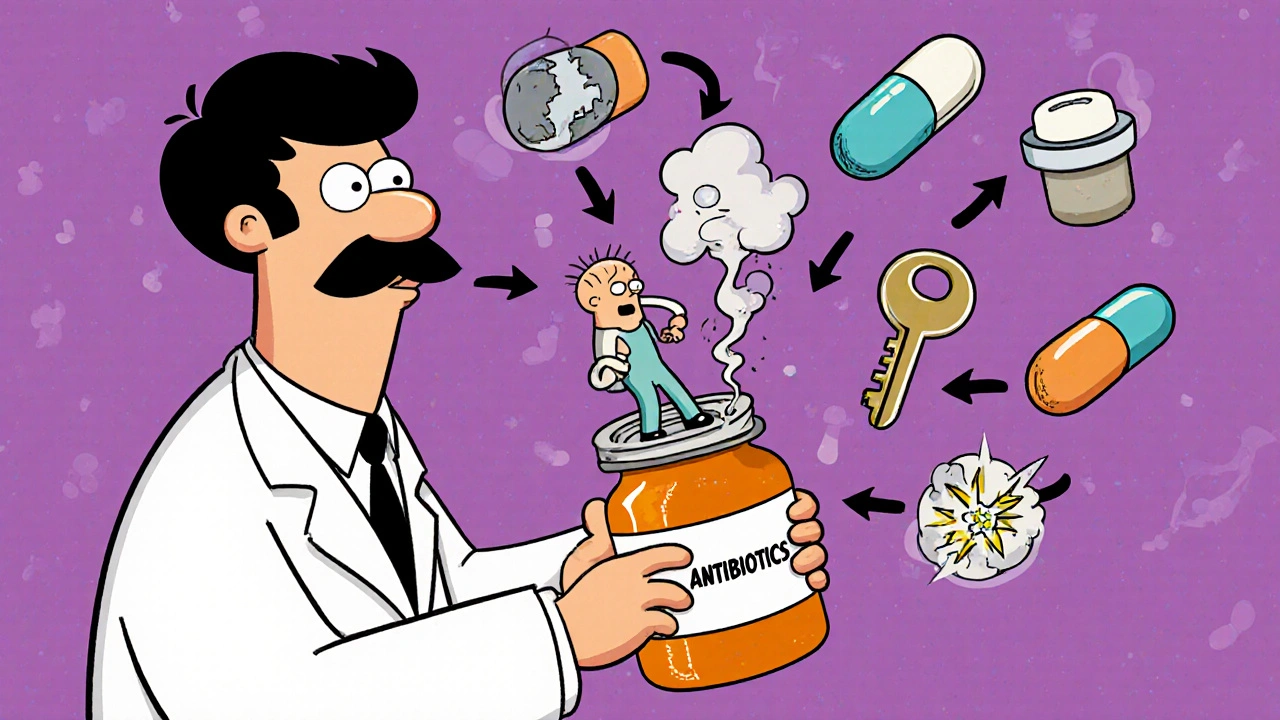
Which Medications Cause Smell Changes?
Over 500 medications are linked to smell and taste disturbances, according to MedLink Neurology’s 2022 update. But not all drugs affect everyone the same way. Some are far more likely to cause problems.
- Antibiotics: Azithromycin, clarithromycin, doxycycline, levofloxacin, and moxifloxacin are top offenders. Fluoroquinolones like levofloxacin and moxifloxacin can chelate zinc-essential for smell cell repair-leading to distortion within days of starting treatment.
- Cardiovascular drugs: Midodrine, used for low blood pressure, has been tied to metallic tastes and phantom smells. It affects nerve signaling in the nose and mouth.
- Neurological medications: Carbamazepine (for seizures) and baclofen (for muscle spasms) can cause complete loss of taste or severe smell distortion. In some cases, patients report food tasting like garbage or chemicals.
- Other culprits: Thyroid meds like carbimazole, diabetes drugs like tolbutamide, and even some antidepressants like sertraline have been shown to interfere with smell receptors.
Some drugs cause instant effects. IV lidocaine or iron infusions can make your mouth taste metallic within seconds. Others take weeks. A 2021 case study in Practical Neurology described a woman who started levofloxacin and, after 10 days, everything she ate tasted like bile. She lost 8 pounds in three weeks.
Why Does This Happen?
Your nose doesn’t just detect smells-it’s a complex chemical lab. Odor molecules bind to receptors in your nasal lining, triggering signals to your brain. Medications can mess with this system in several ways:
- Blocking receptors: Some drugs stop odor molecules from attaching to their targets.
- Overstimulating receptors: Others prevent the receptors from turning off, so signals keep firing even when there’s no smell.
- Disrupting cell function: Antibiotics like doxycycline reduce zinc and magnesium levels, which are needed for smell cells to regenerate.
- Changing nerve signals: Drugs like sertraline can slip into cell membranes and alter how signals are sent to the brain.
It’s not just about taste buds. The olfactory epithelium-the tissue in your nose that detects smells-has cells that turn over every 30 to 60 days. If a drug slows that renewal process, your sense of smell breaks down.
How Long Does It Last?
Most people get better after stopping the drug. The 1995 Schiffman and Nagle study found that 78% of cases resolved within three months. But 22% don’t. Some people struggle for over a year.
Reddit’s r/anosmia community has over 140 posts from people who developed dysosmia after antibiotics. One user, AnosmiaSurvivor92, said they couldn’t eat anything for 22 months because food tasted like rotten eggs. They lost 15% of their body weight.
On the flip side, some recover quickly. A case study in Practical Neurology showed a patient’s taste distortion vanished within five days after switching to mirtazapine, an antidepressant sometimes used off-label for smell recovery.
Why Is This So Often Missed?
Doctors rarely ask about smell changes. A 2022 JAMA Internal Medicine survey found only 37% of primary care doctors routinely check for it during medication reviews. Patients don’t mention it because they think it’s normal or they’re embarrassed.
And here’s the problem: when someone says, “Everything tastes weird,” doctors often jump to neurological causes-Alzheimer’s, Parkinson’s, brain tumors. But in most cases, it’s just a drug side effect. That means people get unnecessary scans, stress, and misdiagnoses.
Dr. Devyani Lal from the University of Arizona says it bluntly: “We don’t ask because we don’t think it matters. But it does. It affects eating, mood, safety-people can’t smell gas leaks or spoiled food.”
What Can You Do?
If you notice smell or taste changes after starting a new medication:
- Don’t stop the drug yourself. Some meds are critical. Talk to your doctor first.
- Write down what changed. When did it start? What smells or tastes are off? Did it happen right after taking the pill?
- Check the list. Look up your medication in the MedLink Neurology database or ask your pharmacist. Many common drugs are on the list.
- Ask about alternatives. Is there another antibiotic or blood pressure pill that doesn’t carry this risk?
- Request a smell test. The University of Pennsylvania Smell Identification Test (UPSIT) is a simple 40-item test that can confirm if your sense of smell is impaired.
Some people try zinc supplements, hoping to fix the problem. But Dr. Thomas Hummel from the University of Dresden warns against it. “Zinc deficiency can cause smell loss, but giving zinc to someone who isn’t deficient won’t help-and can hurt you by causing copper deficiency.”
What’s Being Done About It?
Things are slowly changing. The FDA now encourages drug makers to include smell and taste as endpoints in clinical trials. In 2021, they released draft guidance asking companies to track these side effects more carefully.
The European Medicines Agency plans to require smell and taste assessments in all Phase III trials for antibiotics and heart meds starting in 2024. That’s a big deal-it means future drugs will be tested for this before they hit the market.
Researchers are also testing new treatments. One drug targeting the TRPM5 ion channel (ClinicalTrials.gov NCT05214345) is in Phase II trials. It’s designed to reset the overactive signals causing phantom smells.
Real-Life Impact
It’s easy to think, “It’s just smell.” But losing your sense of smell is like losing a sense of safety, joy, and connection.
People stop eating because food tastes awful. Weight loss, malnutrition, depression follow. One patient in Medindia’s 2023 survey said they couldn’t smell their child’s hair anymore. Another couldn’t detect gas leaks-terrifying for anyone living alone.
Support groups like Fifth Sense in the U.S. and U.K. host monthly virtual meetings for people with drug-induced smell disorders. Over 150 people show up each time. They share stories, coping tips, and hope.
Final Thoughts
Dysosmia isn’t rare. It’s underreported. It’s misunderstood. And it’s often dismissed as “just a side effect.” But if you’re experiencing it, your experience is valid. Your health matters.
If you’re on a medication and your world smells different, don’t brush it off. Talk to your doctor. Ask if it could be the drug. Ask if there’s another option. And if they say it’s not a big deal-ask again. Because sometimes, the smallest change in smell can be the biggest signal that something needs to change.

Alex Harrison
November 6, 2025 AT 01:11I started taking doxycycline for acne and suddenly my coffee tasted like a battery. I thought I was going crazy. Took me weeks to realize it was the drug. Stopped it and after a month it slowly came back. Doctors don’t care until you’re starving.
Jay Wallace
November 6, 2025 AT 16:18Of course it’s the antibiotics. Americans take pills like candy. In my country, we only use meds when absolutely necessary. You people treat your bodies like disposable electronics. Fix your lifestyle before blaming your prescriptions.
Alyssa Fisher
November 7, 2025 AT 09:57This is fascinating because it highlights how little we understand about the olfactory system. Smell isn’t just about receptors-it’s neural mapping, memory association, even emotional conditioning. When a drug disrupts that, you’re not just losing a sense-you’re losing part of your lived experience. The fact that we don’t test for this in trials is a moral failure.
Alyssa Salazar
November 8, 2025 AT 22:57Let’s be real-fluoroquinolones are toxic as hell. They chelate zinc, mess with mitochondrial function, and now we’re finding they fry your olfactory neurons? No wonder people get phantom smells. The FDA should have pulled these decades ago. Pharma’s profit margins shouldn’t outweigh human sensory integrity.
Beth Banham
November 9, 2025 AT 21:49I had this happen after my blood pressure med was switched. Everything smelled like burnt toast. I stopped eating out of sheer dread. Took three months to get better. Just wanted to say-you’re not alone. It’s okay to be upset about this.
Brierly Davis
November 11, 2025 AT 03:10Hey, if you’re going through this, don’t give up. I know it sucks, but I’ve seen people bounce back. Talk to your doc, get the UPSIT test, join a group. Your sense of smell can come back. And if it doesn’t? You adapt. Humans are resilient. You got this.
Amber O'Sullivan
November 11, 2025 AT 12:31My mom lost her smell after sertraline. She cried every time she tried to cook. No one listened until she lost 20 pounds. Now she’s on a different med and it’s slowly improving. Just tell your doctor. Don’t wait
Jim Oliver
November 11, 2025 AT 15:24Wow. Another person blaming Big Pharma. Let me guess-you also think vaccines cause autism and gluten gives you existential dread? Dysosmia is rare. You’re probably just anxious. Stop Googling and go outside.
William Priest
November 12, 2025 AT 14:46Did you know the olfactory epithelium regenerates every 45 days? That’s why most recover. But if you’re still smelling gasoline after 6 months? You’re probably just neurotic. I’ve read all the papers. You’re not special. Just stop obsessing.
Ryan Masuga
November 12, 2025 AT 22:41Been there. Took me 14 months to get my sense of smell back after levofloxacin. I thought I’d never enjoy food again. But I started smelling training-sniffing coffee, citrus, mint every day. It helped. Not a cure, but it gave me hope. You can do this.
Jennifer Bedrosian
November 13, 2025 AT 23:10OMG I thought I was the only one!! I took carbamazepine and suddenly my pasta tasted like dirty socks. I cried in the grocery store. My boyfriend left me because I wouldn’t cook. I’m on mirtazapine now and it’s getting better. I’m alive again. Thank you for writing this
Lashonda Rene
November 15, 2025 AT 16:44I didn’t even know this was a thing until I read this. I’ve been having weird tastes for months and thought it was just stress or aging. I didn’t connect it to my thyroid med. Now I’m gonna ask my doctor about it. Maybe I can fix this. I just want to smell my grandma’s cookies again. That’s all.
Andy Slack
November 17, 2025 AT 14:15Smell is the most underrated sense. It’s tied to memory, safety, joy. If you lose it, you lose part of your soul. This post should be mandatory reading for every med student. Pharma needs to stop treating symptoms and start respecting the whole human.
Rashmi Mohapatra
November 19, 2025 AT 03:01Indian doctors know this. We see it all the time. But you Americans are so obsessed with pills you forget your body is not a machine. Eat turmeric. Stop stress. Don’t take drugs unless you have to. Problem solved.
Abigail Chrisma
November 20, 2025 AT 22:47To the person who said they couldn’t smell their child’s hair-that broke me. I’m a nurse and I’ve seen patients lose their sense of smell after chemo, antibiotics, even SSRIs. We need to normalize asking about it. No one should feel embarrassed for saying "everything smells like death." That’s not weird. That’s medicine failing you.