Medication Smell Risk Estimator
Medication Risk Assessment
This tool helps determine if your medication might be causing smell changes (dysosmia) based on the drug category and symptom timing.
Important: This tool is for informational purposes only. Always consult your healthcare provider before making changes to your medications.
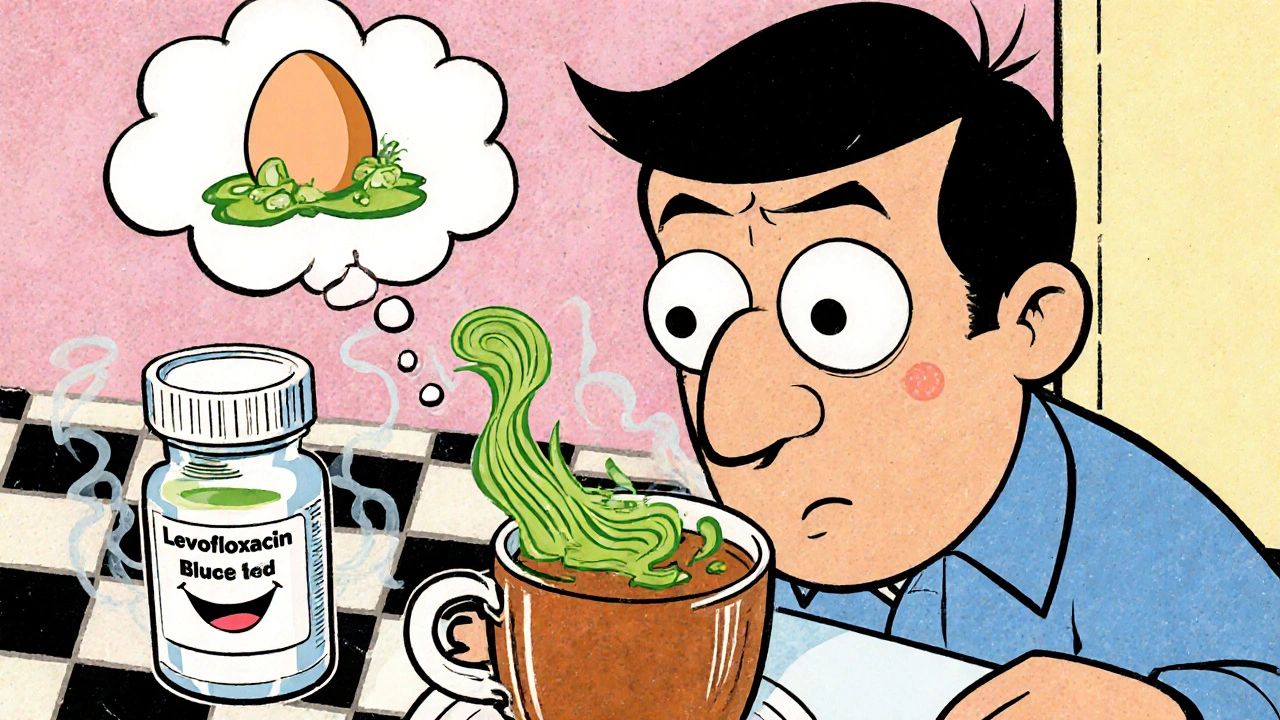
Have you ever taken a medication and suddenly, everything smells wrong? Bread tastes like ash. Coffee smells like burnt rubber. Or worse - you catch a whiff of smoke when no one’s lighting a cigarette? You’re not imagining it. This isn’t just a weird quirk. It’s a real, documented side effect called dysosmia - a distortion in how you perceive smells, often caused by common medications.
What Exactly Is Dysosmia?
Dysosmia means your brain is misreading odor signals. It’s not just losing your sense of smell (that’s anosmia). It’s when familiar scents turn unpleasant, or you smell things that aren’t there. A cup of tea might reek of rotten eggs. Your own breath could smell like metal. Some people report a constant cigarette smoke odor - even in a smoke-free room. This isn’t rare. Over 500 medications are known to cause it, according to MedLink Neurology’s 2022 update. And yet, most doctors don’t ask about it. Patients often assume they’re going crazy, or blame a cold or sinus infection. But if your smell changed after starting a new drug, the timing matters.Which Medications Are Most Likely to Cause Smell Changes?
Some drugs are far more likely to mess with your nose than others. The biggest culprits fall into three categories:- Antibiotics - Especially fluoroquinolones like levofloxacin and moxifloxacin, and macrolides like azithromycin and clarithromycin. These can trigger dysosmia within days. One study found levofloxacin users had 2.5 times higher risk than non-users. The mechanism? They bind to zinc and magnesium in your nasal lining, disrupting the cells that detect smells.
- Cardiovascular drugs - Midodrine, used for low blood pressure, is a known offender. It doesn’t just raise blood pressure - it can alter how your taste and smell receptors fire.
- Neurological and psychiatric drugs - Carbamazepine (for seizures), baclofen (for muscle spasms), and even some antidepressants like sertraline can interfere with the signaling pathways in your olfactory nerves.
Why Does This Happen? The Science Behind the Smell
Your sense of smell relies on delicate cells in your nose called olfactory neurons. These cells have receptors that bind to odor molecules, then send signals to your brain. Medications can mess with this system in several ways:- Blocking receptors - Some drugs physically block odor molecules from binding to their receptors.
- Disrupting signaling - Others interfere with G-proteins, calcium channels, or TRPM5 proteins that help transmit the smell signal.
- Preventing signal shutdown - Normally, smell signals turn off after a few seconds. Some drugs stop this shutdown, causing persistent false signals - like a smell that won’t fade.
- Damaging cells - Antibiotics like doxycycline reduce zinc levels, which are essential for olfactory cell repair. No zinc? No new smell cells. The damage builds up.

How Long Does It Last?
The good news? Most cases get better. The 1995 Schiffman and Nagle study found that 78% of people recover within three months of stopping the medication. But 22% don’t. For some, the distortion sticks around for months - even years. Reddit forums like r/anosmia are full of stories like this: one user took azithromycin for a sinus infection and spent 22 months smelling everything like rotting eggs. Another lost 15% of her body weight because nothing tasted edible. But recovery isn’t guaranteed. Some people need help. Others just wait it out. The key is knowing whether to stop the drug - and when.What Should You Do If You Notice Smell Changes?
Don’t panic. But don’t ignore it either.- Track the timing - Did the smell change start within a week or two of starting a new drug? That’s a strong clue.
- Don’t stop cold - Especially with antibiotics, blood pressure meds, or seizure drugs. Stopping suddenly can be dangerous. Talk to your doctor first.
- Ask about alternatives - If you’re on azithromycin and smell like a garbage dump, ask if another antibiotic is an option. Sometimes switching from levofloxacin to amoxicillin solves the problem.
- Request a smell test - The University of Pennsylvania Smell Identification Test (UPSIT) is a simple 40-item sniff test. It’s not perfect, but it can rule out neurological causes like Parkinson’s or brain tumors.

Are There Treatments?
There’s no magic pill - yet. But some approaches show promise:- Stopping the drug - Still the most effective step. In Medindia’s 2023 survey, 65% of users saw improvement within four weeks of discontinuation.
- Zinc supplements - Sometimes used, but don’t self-prescribe. Dr. Thomas Hummel of the University of Dresden warns that zinc can cause copper deficiency and isn’t proven for drug-induced cases.
- Mirtazapine - An antidepressant that’s been used off-label to treat taste distortion. One case study showed relief in just 4-5 days.
- Future drugs - Clinical trials are testing TRPM5 channel modulators specifically for medication-induced dysosmia (NCT05214345). These could be the first targeted treatments.
Why Is This Underreported?
Because no one asks. Dr. Devyani Lal from the University of Arizona says clinicians rarely bring up smell during medication reviews. Patients don’t think it’s important. Insurance doesn’t cover smell tests. Pharmacovigilance systems don’t track it. The FDA only started encouraging reporting of these symptoms in 2021. Meanwhile, the global market for smell and taste disorders is growing - projected to hit $2 billion by 2030. Pharmaceutical companies are taking notice. AstraZeneca even filed a patent in 2022 for treatments targeting drug-induced smell loss. But for now, the burden falls on you. If you notice a change, document it. Note the drug, the date, and how it affects your eating, mood, and daily life. Bring it to your doctor. Push for answers.What’s Next?
The Global Chemosensory Research Consortium launched a registry in 2023 with over 1,200 patients from 14 countries. The European Medicines Agency plans to require smell and taste assessments in all new antibiotic and cardiovascular drug trials starting in 2024. This is no longer just a nuisance. It’s a public health issue. Poor smell affects nutrition, safety (can you smell gas? smoke?), and mental health. It’s linked to depression and social isolation. You’re not just dealing with a weird smell. You’re dealing with a system that’s ignored your experience for too long. Speak up. Track your symptoms. Ask for help. Your nose - and your health - deserve better.Can antibiotics really change your sense of smell?
Yes. Antibiotics like levofloxacin, azithromycin, and doxycycline are among the most common causes of dysosmia. They interfere with zinc and magnesium in the nasal lining, disrupting smell cell function. Symptoms often appear within 7-14 days of starting the drug.
Will my sense of smell come back after stopping the medication?
In about 78% of cases, smell returns within three months of stopping the medication. But for 22% of people, the distortion lasts longer - sometimes over a year. Early intervention and avoiding further exposure to the drug improve recovery chances.
Is zinc supplementation helpful for medication-induced dysosmia?
Not reliably. While zinc deficiency can cause smell loss, taking extra zinc for drug-induced dysosmia lacks strong evidence. In fact, high doses can lead to copper deficiency and worsen symptoms. Always consult a doctor before supplementing.
Can dysosmia be mistaken for a neurological disorder?
Yes. Persistent smell distortions can mimic early signs of Parkinson’s, Alzheimer’s, or brain tumors. That’s why doctors should rule out neurological causes - especially if symptoms don’t improve after stopping the medication. A smell test like the UPSIT helps differentiate.
What should I do if I can’t smell dangerous odors like gas or smoke?
Install smoke and gas detectors in your home - and check them monthly. Consider using smart alarms that send alerts to your phone. Avoid relying on smell for safety. This is a serious risk, especially for older adults or those on long-term medications.
Are there support groups for people with medication-induced smell changes?
Yes. The nonprofit Fifth Sense runs monthly virtual support groups specifically for people with medication-induced smell and taste disorders. Over 150-200 people participate each month. Online forums like Reddit’s r/anosmia also offer peer support and shared experiences.

Alex Harrison
November 5, 2025 AT 05:51I started taking azithromycin last month and suddenly my coffee tasted like burnt tires. I thought I was going insane until I read this. Took me three weeks to figure out it was the drug. Stopped it and my sense of smell came back in 5 weeks. No one ever asked me about it at the clinic.
Jay Wallace
November 6, 2025 AT 10:55Of course antibiotics mess with your nose-why do you think they’re called ‘broad-spectrum’? They don’t discriminate between good bacteria and the delicate olfactory receptors that evolved over millions of years. This is what happens when you treat every sniffle like a bioterrorism event. The medical-industrial complex is turning people into sensory zombies.
Alyssa Fisher
November 8, 2025 AT 07:10It’s fascinating how something so fundamental as smell-something we take for granted until it’s gone-gets reduced to a footnote in drug inserts. We prioritize efficacy and side effects like nausea or dizziness, but not the collapse of your emotional connection to food, memory, or safety. Smell isn’t just a sense; it’s a bridge to your past. When it breaks, you grieve in silence.
Alyssa Salazar
November 8, 2025 AT 18:37TRPM5 channel modulators are the future-this isn’t just anecdotal, it’s pharmacological. The olfactory epithelium is a neuroepithelial interface, and drugs like fluoroquinolones are literally hijacking calcium signaling cascades. We need clinical trials with olfactory event-related potentials, not just self-reports. Also, mirtazapine’s off-label use is underexploited-serotonin 5-HT2C antagonism may reset aberrant neural firing patterns in the piriform cortex. Someone’s gotta fund this.
Beth Banham
November 10, 2025 AT 10:53I had this happen after my iron infusion. Everything smelled like pennies for six months. I stopped eating because I couldn’t stand the taste. I didn’t tell anyone because I thought it was just me. Reading this made me feel less alone. Thank you for writing this.
Brierly Davis
November 11, 2025 AT 17:31If you’re on a med and your world smells like garbage, don’t suffer in silence. Talk to your doctor. Bring this article. Ask for alternatives. You’re not being dramatic-you’re being smart. And if they blow you off, go to a different doctor. Your nose matters. Your life matters.
Amber O'Sullivan
November 11, 2025 AT 19:33My sister took levofloxacin and smelled smoke for 14 months. No one believed her. She lost 20 pounds. She cried every time she tried to cook. The system fails people like her every day
Jim Oliver
November 13, 2025 AT 14:07Wow. Someone finally admitted that doctors are negligent. Took long enough. Also, zinc supplements? Please. You’re not a 1990s nutrition guru. This isn’t a deficiency-it’s a pharmacological assault. And no, you don’t get to ‘wait it out’ if you’re a diabetic who can’t smell insulin leaks.
William Priest
November 14, 2025 AT 11:42Let me guess-you got this from Reddit and now you think you’re a neurologist? The UPSIT test is garbage. It’s not standardized across populations. And mirtazapine? That’s just sedating the brain, not fixing the receptor damage. You’re all just vibing with anecdotal evidence while real science gets ignored.
Ryan Masuga
November 14, 2025 AT 15:04Hey, if you’re reading this and you’re going through this-don’t give up. I was there. Took me 8 months. Found a new doc who actually listened. Switched from levofloxacin to amoxicillin. Smell came back slowly but it came back. You’re not broken. The system is just slow. Keep pushing. You got this.