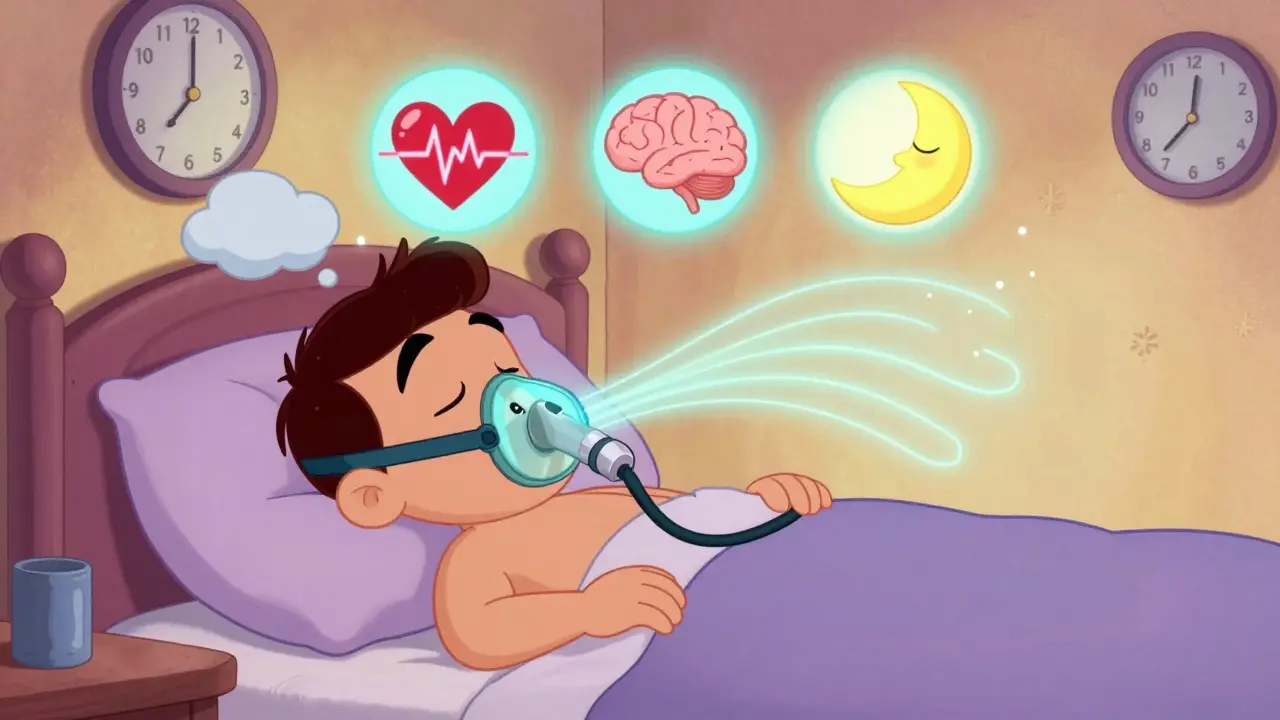
Obstructive sleep apnea isn’t just about snoring. It’s when your throat muscles relax too much during sleep, blocking your airway and causing you to stop breathing-sometimes dozens of times an hour. You might not even remember it, but your body does. Your oxygen drops. Your heart races. You jerk awake just enough to breathe, then fall back into the same cycle. Over time, this wears down your body. High blood pressure, heart disease, brain fog, and daytime exhaustion aren’t just side effects-they’re direct results. And if you’ve been told you have it, you’re not alone. About 1 billion people worldwide live with this condition.
CPAP: The Gold Standard, But Not Perfect
For more than 40 years, CPAP has been the go-to treatment. It works by pushing a steady stream of air through a mask to keep your airway open. No surgery. No pills. Just air pressure. The first device was invented right here in Australia in 1981, and today’s models are smarter, quieter, and lighter than ever. Most weigh less than 3 pounds and run as quietly as a whisper.
There are three main types: standard CPAP delivers one fixed pressure, auto-CPAP (or APAP) adjusts pressure automatically based on your breathing, and BiPAP gives you different pressures for inhaling and exhaling. For most people with moderate to severe sleep apnea, CPAP cuts apnea events from 30+ per hour down to under 10-sometimes even under 5. That’s not just better sleep. That’s fewer heart attacks, lower blood pressure, and sharper thinking.
But here’s the catch: it only works if you use it. A 2020 study found that people who wore their CPAP for 7+ hours a night saw dramatic improvements. But those who used it for less than 4 hours? They still had moderate to severe sleep apnea-even while using the machine. And that’s the problem. About half of people stop using CPAP within the first year. Why? Mask discomfort. Dry mouth. Claustrophobia. Leaks. Noise. Travel hassle.
One user on Reddit said, “I’ve tried five masks over two years and still can’t get past two hours.” Another said, “Switched to a nasal pillow mask-now I sleep 7+ hours. My daytime tiredness dropped in half.” It’s not about the machine. It’s about finding the right fit.
Oral Appliances: A Simpler, More Comfortable Option
If CPAP feels like a battle, oral appliances might be your answer. These are custom-fitted devices, like mouthguards, that gently move your lower jaw forward to keep your airway open. They’re small, quiet, and easy to pack. No hoses. No electricity. Just pop it in before bed and sleep normally.
They’re not as powerful as CPAP for severe cases-but they’re far more popular in the long run. A 2017 review found that people used oral appliances on 77% of nights after a year. CPAP? Only 4 to 5 hours a night on average. That’s not a small difference. That’s the difference between treatment and no treatment.
Studies show that while CPAP brings AHI (apnea events per hour) down to 4.7 when used well, oral appliances bring it down to around 10-15. For mild to moderate cases, that’s often enough. And for people who can’t tolerate CPAP? It’s a lifeline. Many dentists now offer sleep apnea appliances as part of routine care. Insurance often covers them, especially if CPAP failed.
They’re not perfect either. Some users report jaw pain, tooth movement, or saliva issues. But for many, the trade-off is worth it. If you value comfort, portability, and consistency over maximum power, this is the alternative that works.
Surgery and Implants: For the Right Candidates
Surgery sounds like a permanent fix, but it’s rarely that simple. UPPP-removing excess tissue from the throat-has a success rate of only 40-60%. That means nearly half the people who go under the knife still need CPAP afterward. Tonsil removal helps if you have large tonsils. Nasal surgery can improve airflow, but it won’t fix the root issue if your tongue collapses backward.
Then there’s Inspire therapy. It’s a small implant placed in your chest that stimulates the nerve controlling your tongue. When you sleep, it gently moves your tongue forward to keep your airway open. Sounds futuristic? It is. And it works-79% reduction in apnea events on average. But it costs around $35,000 out-of-pocket. It requires surgery. And it’s only approved for people who can’t use CPAP and have moderate to severe apnea. It’s not a first-line option. It’s a last-resort option for a small group.
Who Benefits Most from CPAP? And Who Should Look Elsewhere?
Not everyone responds the same way to CPAP. New research from Harvard, Stanford, and Yale shows it’s not just about severity-it’s about your brain’s arousal threshold. Think of it like this: some people wake up easily at the first sign of trouble. Others sleep through it. If you’re the kind who wakes up easily, CPAP feels like a miracle. You feel more alert, think clearer, and your blood pressure drops. But if your brain ignores the breathing interruptions, CPAP might not change how you feel at all.
That’s why experts now say: don’t just treat the numbers. Treat the person. If you’ve tried CPAP and still feel exhausted, it might not be the machine. It might be your biology. In those cases, oral appliances, weight loss, or positional therapy (sleeping on your side) might work better.
Positional therapy devices, like the NightBalance belt, vibrate gently when you roll onto your back. For people whose apnea only happens when they sleep on their back (about 50% of cases), this reduces events by over 50%. No mask. No pressure. Just a gentle nudge.
Getting Started: What You Really Need to Know
You can’t just buy a CPAP machine online. You need a diagnosis first. That means either a sleep lab test or a home sleep test. Once you know your AHI, your doctor will recommend a treatment path. If you’re prescribed CPAP, don’t expect to master it overnight. Most people need 2-4 weeks to adjust.
Start slow. Wear the mask for an hour while watching TV. Then two hours. Then overnight. Use a humidifier if your nose feels dry. Try a nasal pillow mask if the full-face feels too much. Chin straps help if you breathe through your mouth. Clean your mask daily. Wash the tubing weekly.
And don’t give up after a bad week. Most people who stick with it past 90 days become consistent users. ResMed’s data shows 97% of patients complete their first month visit. 84% make it to six months. The key? Support. If your DME provider doesn’t call you back within 24 hours, switch. If your sleep clinic doesn’t offer follow-up visits, ask for one. You’re not failing. The system is just not built for you yet.

The Future Is Personalized
The next big shift isn’t a new machine. It’s smarter matching. In 2024, guidelines are expected to start recommending treatment based on arousal threshold, not just AHI. If your brain ignores apneas, CPAP won’t help much. If you’re a light sleeper, CPAP could change your life. That’s why future devices will use AI to analyze your breathing, snoring, and even heart rate to adjust pressure in real time.
Apps like Nightware, recently cleared by the FDA, use biofeedback to help you fall asleep faster and stay asleep longer-boosting CPAP adherence by 22%. 3D imaging of your airway is now being used to design custom oral appliances that fit perfectly. We’re moving from one-size-fits-all to one-size-fits-you.
But here’s the truth: no treatment works unless you use it. CPAP is powerful. Oral appliances are practical. Surgery is risky. Positional therapy is simple. The best treatment isn’t the most advanced one. It’s the one you’ll actually wear every night.
Is CPAP the only treatment for obstructive sleep apnea?
No. While CPAP is the most effective treatment for moderate to severe cases, it’s not the only option. Oral appliances, positional therapy devices, weight loss, and in rare cases, surgery or nerve implants, are all valid alternatives. The best choice depends on your severity, anatomy, lifestyle, and how well you tolerate each option.
Why do so many people stop using CPAP?
Mask discomfort, dry nose or mouth, claustrophobia, noise, and difficulty traveling are the top reasons. Studies show 50% of users stop within the first year. Many find oral appliances more comfortable. Others improve with better mask fit, humidification, or gradual acclimation. It’s not laziness-it’s often a mismatch between the device and the person.
Can I use an oral appliance instead of CPAP?
Yes-if you have mild to moderate obstructive sleep apnea, or if you can’t tolerate CPAP. Oral appliances are FDA-cleared and covered by many insurance plans. They’re less effective for severe cases, but they have much higher long-term use rates. Many patients switch from CPAP to an oral appliance and report better sleep quality because they actually wear it.
Does losing weight help with sleep apnea?
Absolutely. Excess weight, especially around the neck, increases airway collapse. Studies show that losing just 10% of body weight can reduce apnea events by up to 50%. For some people, weight loss alone can eliminate the need for any device. It’s not a quick fix, but it’s one of the most effective long-term strategies.
How do I know if my CPAP is working?
Check your machine’s data. Most modern devices track usage hours, residual apnea events (AHI), and leak rates. If you’re using it 6+ hours a night and your AHI is under 5, it’s working. You should also notice less snoring, fewer morning headaches, and more energy during the day. If you’re still tired, talk to your sleep specialist-you might need a pressure adjustment or a different mask.
Are there any new treatments on the horizon?
Yes. Future treatments are moving toward personalization. Devices will soon use AI to adjust pressure based on your unique breathing patterns. 3D airway scans will help design custom oral appliances. Apps are being developed to improve sleep onset and adherence. And research is underway into medications that strengthen upper airway muscles during sleep. But for now, the best treatment is still the one you’ll actually use.
What to Do Next
If you’ve been diagnosed with obstructive sleep apnea, don’t panic. Start by understanding your numbers: what’s your AHI? Are you a mouth breather? Do you sleep on your back? Do you feel rested after a full night? Then explore your options-not just CPAP. Talk to a sleep specialist, ask about oral appliances, try a positional device, or consider weight loss. You don’t have to accept discomfort as part of treatment. The goal isn’t just to reduce events-it’s to restore your life.


Bradford Beardall
January 11, 2026 AT 11:05McCarthy Halverson
January 13, 2026 AT 07:23lisa Bajram
January 14, 2026 AT 12:37Christine Milne
January 15, 2026 AT 00:04Michael Marchio
January 15, 2026 AT 06:40Ashlee Montgomery
January 17, 2026 AT 02:58neeraj maor
January 17, 2026 AT 03:52Ritwik Bose
January 18, 2026 AT 04:06Paul Bear
January 19, 2026 AT 15:39Kunal Majumder
January 20, 2026 AT 12:37Aurora Memo
January 21, 2026 AT 03:37Jaqueline santos bau
January 21, 2026 AT 18:58McCarthy Halverson
January 22, 2026 AT 00:34