Getting the right dose of liquid medicine isn’t just important-it can be life-or-death. Especially for kids, seniors, and people with chronic conditions, a tiny mistake in measurement can mean the difference between healing and hospitalization. According to a 2023 study in the Journal of Pediatrics, about 80% of pediatric home medication errors involve liquid medications. That’s not a small number. It’s a system-wide problem. And the worst part? Most of these errors are completely preventable.
Why Liquid Medications Are So Risky
Liquid medications are tricky because they’re measured in tiny amounts-sometimes less than a single drop. A prescription for 2.5 mL might sound simple, but if you’re using a kitchen spoon, a dosing cup with blurry markings, or you misread "tsp" as "tbsp," you’re already off track. The Institute for Safe Medication Practices lists wrong-dose liquid errors as one of the top 10 persistent medication hazards in 2024. And it’s not just parents making mistakes. Nurses, pharmacists, and doctors all contribute to the problem.
Here’s what goes wrong:
- Using household spoons: A tablespoon isn’t 15 mL-it’s often closer to 18 mL. That’s a 20% overdose right there.
- Confusing "mL" with "tsp" or "tbsp": Even if the label says "2 mL," caregivers often assume it means "2 teaspoons."
- Look-alike bottles: Two different medicines in similar bottles with similar labels can be swapped by accident.
- Bad measuring tools: Dosing cups are notoriously inaccurate. A 2021 study in Academic Emergency Medicine found error rates of 41% with dosing cups for doses under 5 mL.
- Lack of training: Many caregivers aren’t shown how to use an oral syringe properly. They’re handed a cup and told to "give it as directed."
The consequences? Treatment failure, vomiting, drowsiness, seizures, even death. A 2022 New England Journal of Medicine study found that hospitals using full safety bundles reduced serious errors by 67% in just 18 months. That’s not magic-it’s consistency.
The One Tool That Makes All the Difference: The Oral Syringe
If you remember only one thing from this guide, remember this: Always use an oral syringe for liquid medications.
Oral syringes aren’t just better-they’re the gold standard. The American Academy of Pediatrics has recommended them since 2015. Why? Because they’re precise. A 2016 Yale study found oral syringes are 37% more accurate than dosing cups. NIH testing in 2022 showed 94% accuracy for a 2.5 mL dose with a syringe, compared to just 76% with a cup and 62% with a household spoon.
Here’s how to pick the right one:
- For doses under 1 mL: Use a 1 mL syringe with 0.1 mL markings. These let you measure 0.3 mL, 0.7 mL-exactly.
- For doses between 1 and 5 mL: Use a 5 mL syringe with 0.5 mL markings. No more guessing.
- Never use a syringe with an IV tip. Always look for "oral use only" or "for mouth."
Pharmacies should hand you one with every liquid prescription. If they don’t, ask for it. It’s not a luxury-it’s a safety requirement. The American Academy of Family Physicians has recommended syringe-only distribution for pediatric meds since 2020. And yet, a 2023 HealthyChildren.org survey found only 54% of caregivers actually received one.
Stop Using Teaspoons and Tablespoons-Ever
"Give two teaspoons" is a dangerous phrase. Why? Because a teaspoon isn’t a standardized unit. In the U.S., it’s 4.93 mL. In the U.K., it’s 5 mL. In Australia, it’s 5 mL. But a kitchen spoon? It varies from 3 mL to 10 mL depending on the spoon, the person, the day.
The World Health Organization says eliminating non-metric units is the single most effective way to cut wrong-dose errors-preventing 33% of them. Dr. Michael Cohen of ISMP says teaspoons and tablespoons account for 28% of preventable pediatric errors every year.
Here’s what you need to see on every prescription and bottle:
- Only "mL"-never "tsp," "tbsp," "cc," or "drops."
- Clear, bold font.
- "FOR ORAL USE ONLY" in capital letters.
Pharmacies must follow ANSI Z535.4-2011 safety label standards. If you see "teaspoon" on the label, refuse the medication. Ask for a new label. Your life depends on it.

How Hospitals and Pharmacies Are Fixing This
It’s not just up to caregivers. The system has to change too.
Since 2016, the International Organization for Standardization has required all enteral (tube-feeding) connectors to use the ENFit system. This means liquid medications for feeding tubes can’t accidentally connect to IV lines. Hospitals that switched to ENFit saw wrong-route errors drop by 98%. That’s huge.
Electronic prescribing (e-prescribing) systems with built-in clinical decision support are another game-changer. If a doctor tries to prescribe 10 mL of a medicine for a 10-pound baby, the system should flash a warning. A 2023 Cochrane Review found these systems cut pediatric liquid errors by 58%.
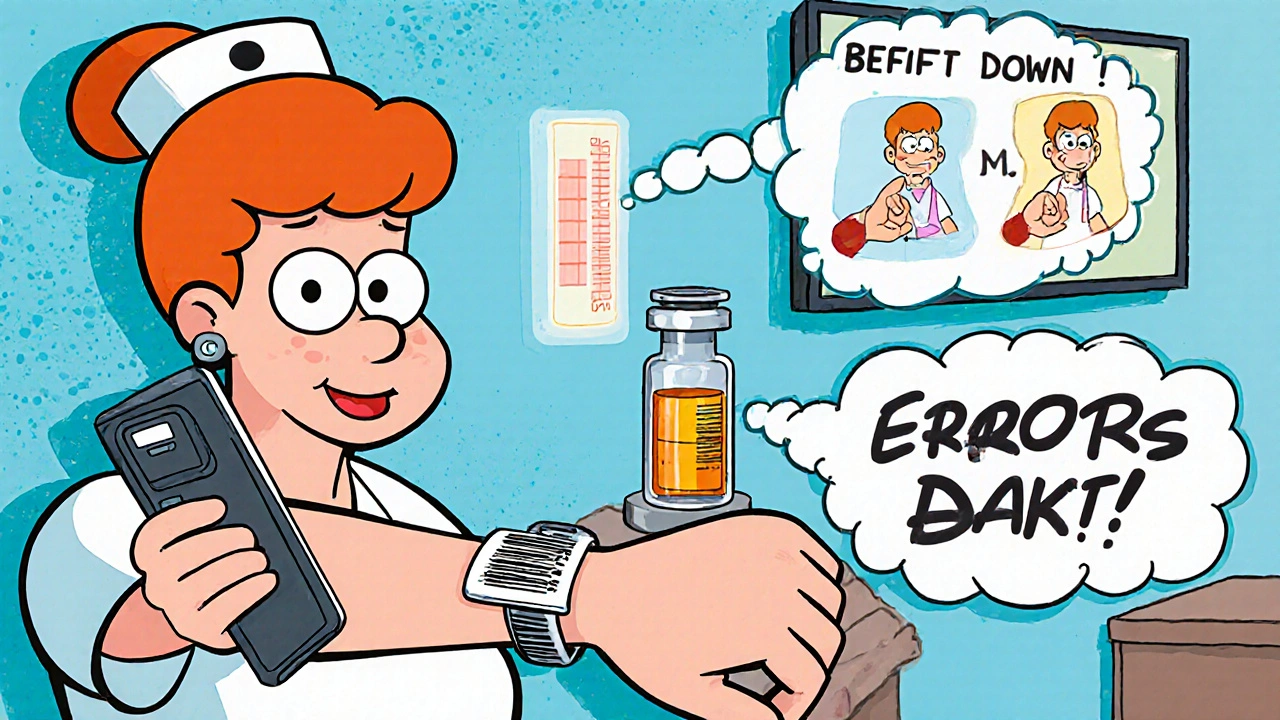
Barcode medication administration (BCMA) systems-where nurses scan the patient’s wristband and the medication before giving it-reduce errors by 48%. But only if used 100% of the time. If someone skips the scan, the safety net breaks.
And then there’s repackaging. Medications should come in amber bottles with bold labels. Look-alike packaging causes 49% of nursing errors, according to AllNurses.com. Standardized packaging cuts those errors by 42%.
But here’s the catch: Only 42% of U.S. hospitals have fully adopted ENFit. Only 48% verify staff competency in dosing. And 84% of rural clinics say cost is a barrier. Change is slow-but it’s happening.
What You Can Do at Home
You don’t need fancy tech to keep your family safe. Here’s your action plan:
- Always ask for an oral syringe when a liquid medication is prescribed. If they say no, ask why.
- Throw away dosing cups. They’re outdated and inaccurate.
- Write down the dose in mL. Put it on your phone, on the fridge, on the bottle itself.
- Never use kitchen spoons. Ever.
- Double-check the label: Is it mL? Is it for oral use? Is the dose right for the person’s weight?
- If you’re unsure-call the pharmacy. Don’t guess.
- Keep all medications out of reach and in their original containers. Never transfer to another bottle.
- Use a light-colored background when measuring. A white counter makes it easier to see the liquid level.
Some pharmacies now offer pre-measured, single-dose syringes. These cost a bit more, but they’re 94% accurate and eliminate all measurement risk. If your pharmacy offers them, take them. It’s worth it.
What to Do If You Made a Mistake
Everyone makes mistakes. If you gave the wrong dose, don’t panic-but don’t ignore it either.
- If you gave too little: Don’t double the next dose. Call your provider. They’ll tell you what to do.
- If you gave too much: Call Poison Control immediately (1-800-222-1222 in the U.S.). Even if your child seems fine, some effects take hours to show.
- Write down what happened: What medicine? What dose? What device did you use? When? This helps your doctor assess risk.
- Report it to your pharmacy. They need to know so they can improve.
One parent on Reddit shared that after giving her toddler 10 mL instead of 2 mL of amoxicillin, she called Poison Control. They said to watch for vomiting or drowsiness. She did-and nothing happened. But she didn’t know that unless she called. Don’t wait.
The Future Is Here
Technology is catching up. The FDA’s 2024 draft guidance requires all over-the-counter liquid medicines to include an enclosed dosing device that meets ASTM F3100-23 standards-meaning they must have metric markings and safe connectors.
Smartphone apps are being tested at Boston Children’s Hospital. Point your phone at the bottle, and an AR app shows you exactly where the liquid should be for the correct dose. At Johns Hopkins, RFID-tagged syringes send dose data directly to the EHR. Pilot results? 89% fewer errors.
By 2026, all certified electronic health records in the U.S. must include automatic pediatric dose checking. That’s a big step.
But none of this matters if caregivers aren’t educated. The most effective tool isn’t a syringe or a barcode scanner-it’s knowledge. And that’s something you can start using today.
Final Reminder
Medication safety isn’t about being perfect. It’s about being consistent. It’s about asking for the right tool. It’s about saying no to teaspoons. It’s about double-checking.
Wrong-dose errors are preventable. Not because of fancy tech. But because we choose to do better. Start today. Ask for the syringe. Write down the mL. Trust no spoon. Your family’s health depends on it.



Kara Binning
November 19, 2025 AT 05:41This is why America’s healthcare system is broken. They hand you a cup with blurry markings and expect you to be a pharmacist? I’ve seen my neighbor give her kid medicine with a soup spoon-because the pharmacy "didn’t have syringes in stock." And now she’s blaming the mom? No. The system failed her. And it’s failing everyone.
river weiss
November 19, 2025 AT 19:27It is imperative to emphasize that the use of oral syringes for liquid medication administration is not merely a recommendation-it is a clinical best practice, supported by extensive empirical evidence from peer-reviewed studies conducted by Yale, the NIH, and the AAP. The variance in household spoon volumes, coupled with the absence of standardized labeling, constitutes a systemic risk factor that must be addressed at both the provider and policy levels. I urge all caregivers to request syringes at point of dispensing, and to refuse any formulation that does not include metric-only labeling.
Frank Dahlmeyer
November 21, 2025 AT 11:57Let me tell you something-I used to be the guy who just grabbed a kitchen spoon because it was easy, you know? I thought, "It’s just a little more, what’s the harm?" Until my niece had a seizure after I gave her too much ibuprofen because I confused mL with tsp. That’s when I realized-this isn’t about being careful. It’s about being educated. Now I keep five oral syringes in my medicine cabinet, labeled for each kid. I even bought a little box from Amazon that holds them with the meds. I don’t care if it looks weird-I’d rather look weird than bury a child. And if your pharmacy doesn’t hand you one? Walk out. Go to another one. This isn’t negotiable. Your kid’s life isn’t a suggestion.
Reema Al-Zaheri
November 22, 2025 AT 12:12While the emphasis on oral syringes is commendable, it is equally critical to address the linguistic ambiguity inherent in pharmaceutical labeling. The continued use of non-metric units-even in informal contexts-perpetuates cognitive dissonance among caregivers who are not medically trained. Furthermore, the absence of standardized font size, contrast ratios, and tactile markings on bottles renders these labels inaccessible to visually impaired users. The WHO’s recommendation to eliminate non-metric units is not merely prudent-it is a human rights imperative.
Derron Vanderpoel
November 22, 2025 AT 21:07Okay I just want to say I DID THIS. I gave my 2-year-old 10ml instead of 2ml of amoxicillin because I was tired and the bottle looked the same as the other one. I panicked. I called poison control. They said "watch for vomiting or drowsiness." I sat there with her for 8 hours. She was fine. But I cried for 3 hours. Please. Please. Please. Just use the syringe. I didn’t want to be that parent. I didn’t even know I could be that parent. I am so sorry.
Timothy Reed
November 24, 2025 AT 01:58The data presented here is robust and aligns with current clinical guidelines. The adoption of ENFit connectors and barcode medication administration systems has demonstrated measurable reductions in error rates across multiple institutional settings. However, implementation barriers-including cost, staffing, and training-remain significant, particularly in rural and under-resourced clinics. A multi-stakeholder approach involving pharmacists, clinicians, policymakers, and caregivers is essential to scale these interventions effectively.
Christopher K
November 25, 2025 AT 16:30Oh wow. A whole article about how to use a syringe? And you think this is news? We’ve had these since the 1980s. The real problem isn’t the spoon-it’s the people who think they’re too busy to read the label. Or worse, the doctors who still write "tsp" on prescriptions. If you can’t read mL, maybe don’t parent. Just sayin’.
harenee hanapi
November 27, 2025 AT 09:52Everyone’s so quick to blame caregivers, but let’s be real-pharmacies are the ones who refuse to give out syringes. They say it’s "too expensive" or "not standard." But they’ll give you 50 plastic bags and 3 different kinds of napkins for your coffee. Why won’t they give you a $0.25 syringe to save a child’s life? I’ve been told "we don’t stock them" 7 times. I’ve cried in 3 pharmacies. No one cares. It’s not about the spoon. It’s about who gets to live and who gets to be ignored.
Andy Feltus
November 27, 2025 AT 19:27It’s funny how we’ve turned medicine into a precision engineering problem when it’s really a human one. We’ve got AR apps and RFID syringes and FDA guidelines-but the real solution is still the same: slow down. Ask. Double-check. Admit you’re scared. That’s the technology no one talks about. The one that doesn’t cost a dime. The one that requires you to be vulnerable enough to say, "I don’t know." And maybe that’s the hardest thing of all.
Brian Rono
November 28, 2025 AT 04:24Oral syringes? Please. That’s just the tip of the iceberg. What about the fact that 80% of liquid meds are prescribed in hospitals where nurses still use measuring cups? What about the fact that the FDA allows "cc" on labels? What about the fact that some brands still use red caps for sedatives and blue for antibiotics-when red means danger and blue means calm? This isn’t a care issue. It’s a design failure. And someone’s getting paid to keep it this way.
seamus moginie
November 30, 2025 AT 04:15My brother-in-law is a pharmacist in Cork-he says they’ve been giving out syringes with every liquid script since 2018. No questions asked. The government subsidizes them. No one complains. Meanwhile, in the States, people are still using tablespoons like it’s 1950. It’s not a cultural difference. It’s a political failure. You can fix this. You just need to care enough to demand it.
Dana Dolan
December 2, 2025 AT 03:18I just got my kid’s new antibiotic. Pharmacy gave me a syringe. I didn’t even ask. I just smiled and said thanks. I’m not a hero. I’m just tired of being scared. This is the small thing we can all do. Ask. Use it. Don’t apologize for it.
Steve and Charlie Maidment
December 3, 2025 AT 16:44Look, I get it. Syringes are better. But let’s be honest-most people don’t have the time, energy, or mental bandwidth to micromanage every drop of medicine. You think I want to sit there with a 1 mL syringe and count 0.7 mL while my kid screams? No. I want the pharmacy to just give me a pre-filled, single-dose cup that’s accurate. Or better yet-make the medicine solid. Why are we still doing this in 2024? It’s archaic. And now you’re making guilt-trip parents feel bad for not being perfect? That’s not helping. That’s just adding stress.
Michael Petesch
December 4, 2025 AT 12:12As someone who has worked in pediatric clinics across five countries, I can confirm that the cultural perception of medication measurement varies widely. In India, for example, many caregivers rely on traditional units like "dose" or "pinch," which are not standardized. The challenge is not only technical but deeply cultural. Education must be localized, linguistically appropriate, and delivered through trusted community figures-not just pamphlets from pharmacies.
Ellen Calnan
December 4, 2025 AT 21:38I used to think this was overkill-until my daughter had a reaction to a 10% overdose of her seizure med. She was fine. But I lost three days of sleep. I started keeping a notebook: medicine name, dose in mL, device used, time given, and how she looked after. I took pictures of the syringe level. I made a chart. I became obsessed. Because I realized-safety isn’t a checklist. It’s a habit. And habits are built one tiny, terrifying, careful moment at a time. I still panic when I open the cabinet. But now I know: I’m not crazy for being careful. I’m the only one who’s paying attention.