If you've got a drug-eluting stent or know someone who does, understanding the risks can be a lifesaver—literally. Drug-eluting stents have been a game-changer, slowly releasing medication to prevent arteries from narrowing again. But they're not completely risk-free. Blood clots can, and do, form and cause complications. So, what's the deal with these blood clots? Let's break it down.
One of the sneaky things about blood clots is they sound like something only the experts can understand, but they're not really. Basically, your body's clotting response is essential for healing, but when you have a stent in your artery, it can overreact. The stent's metal framework can irritate the arterial wall, and the body's healing process can lead to clots.
Are the benefits of these stents worth the risk? In many cases, yes. But it's crucial to have a chat with your doctor about your personal risks and benefits before making decisions. Remember, these aren't blanket solutions for everyone. We'll dig more into this as we go.
Want to lower your risk of these pesky clots? Keep up with medications like blood thinners which your doctor might prescribe. And, you know, the same old advice still rings true: eat well, stay active, and quit smoking! It's boring but works wonders. Regular check-ups can keep you in the loop and help catch any sneaky problems early.
- What are Drug-Eluting Stents?
- How Do Blood Clots Form?
- Balancing Risks and Benefits
- Practical Tips and Prevention Strategies
What are Drug-Eluting Stents?
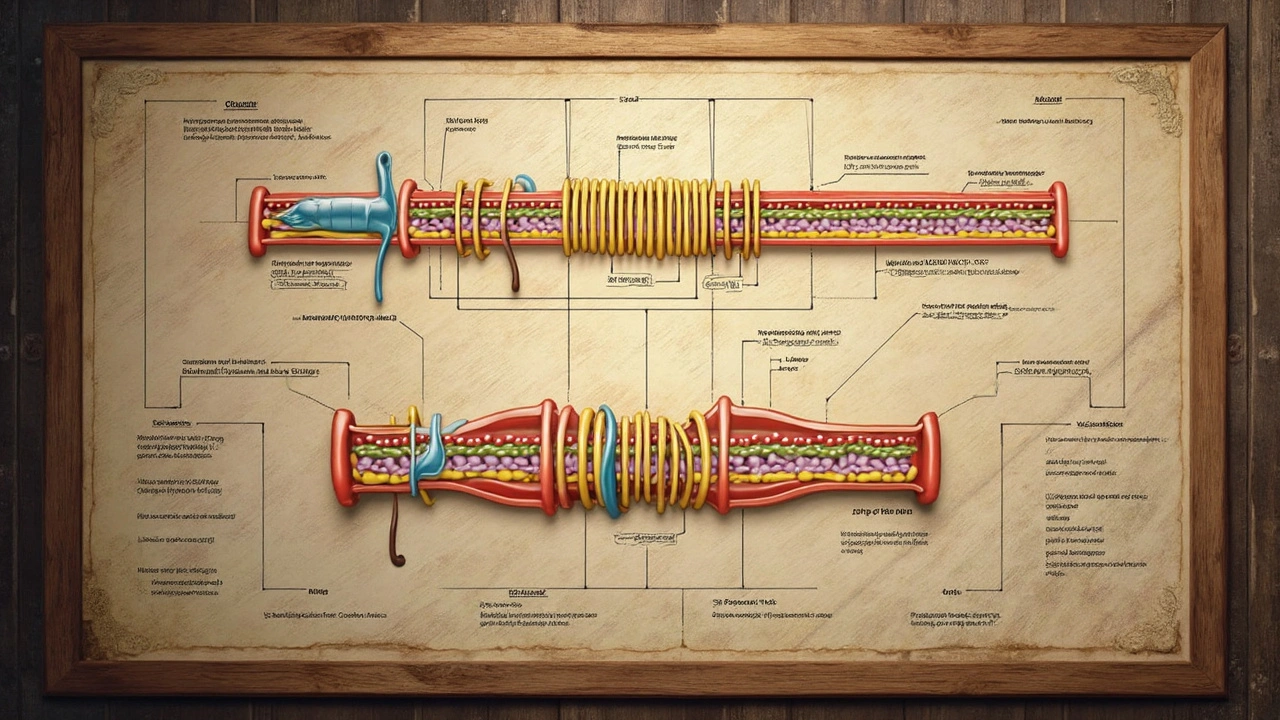
Ever heard of drug-eluting stents and wondered what the buzz is about? These little devices have made quite a splash in the cardiac world. So, what are they exactly? Well, think of them as tiny scaffolds placed inside your coronary artery to prop it open. But there's more to them than meets the eye.
Unlike traditional stents, drug-eluting stents are coated with medication that slowly seeps into the arterial wall. This medicine helps prevent the artery from getting narrow again, a condition doctors refer to as restenosis. And what's in this special coating? It's often drugs like sirolimus or paclitaxel, known for slowing down cell growth.
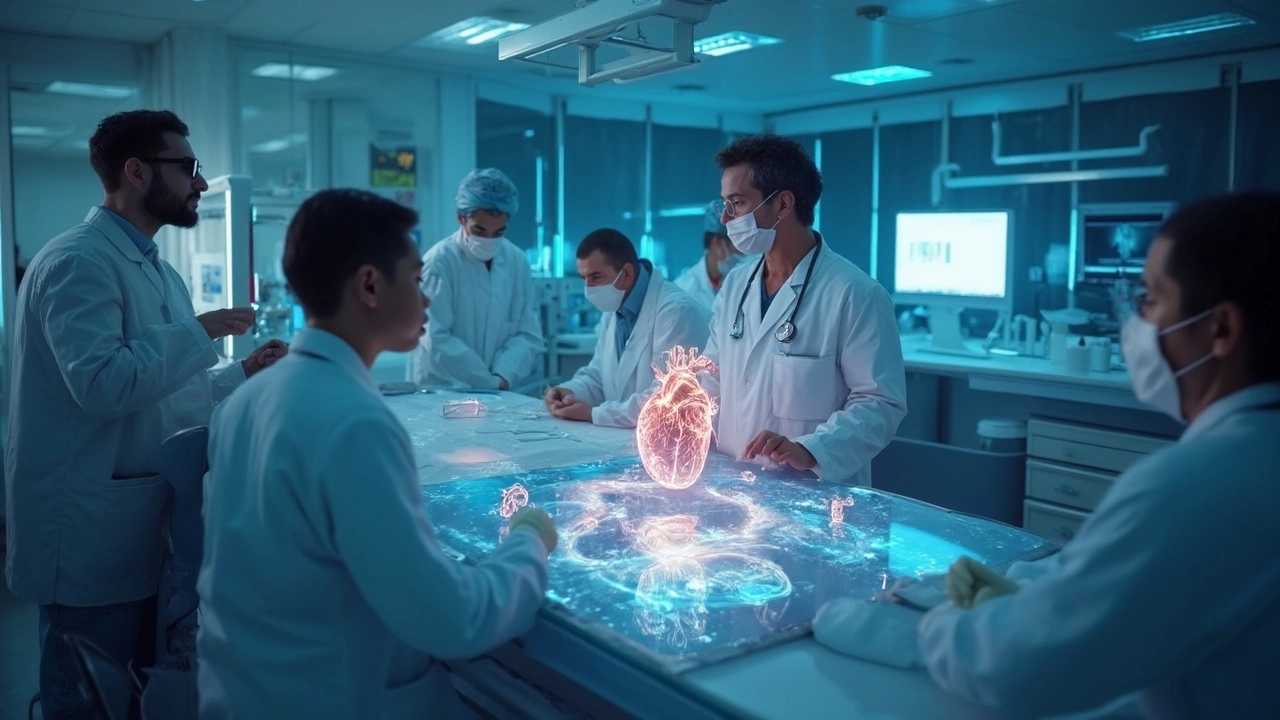
"The development of drug-eluting stents has significantly reduced the incidence of restenosis, making them a key tool in modern cardiology," says Dr. Alexandra Leaf, a leading cardiologist at Heart & Health Institute.
So, how do they work their magic? After the stent is placed during a procedure called angioplasty, it gradually releases the medication over a few months. This keeps the artery open long enough for it to heal properly without scar tissue causing trouble.
Big facts you might want to know: drug-eluting stents have been shown to reduce the risk of restenosis by almost 70% compared to bare-metal stents. But, they're not a one-size-fits-all solution. They require a longer-term commitment to blood-thinning medications, like aspirin and clopidogrel, to prevent those sneaky blood clots we talked about earlier.
Have a peek at some basic data on drug-eluting stents compared to their predecessors:
| Type of Stent | Restenosis Rate | Clot Risk |
|---|---|---|
| Bare-Metal Stent | 20-30% | Lower |
| Drug-Eluting Stent | 5-10% | Higher |
These bad boys have certainly changed the game in treating coronary artery disease. But like all good things, they come with their caution flags. Make sure to chat in-depth with your healthcare provider to see if drug-eluting stents are your best rush towards a healthier heart.
How Do Blood Clots Form?
So, you're wondering how exactly a blood clot turns up in a stent. Let's break it down. When you get a stent, especially a drug-eluting stent, it's like an invader in your artery. The stent itself has a metal scaffold, and your body isn't always a fan of foreign bodies hanging around.
Here's what happens: after a stent is implanted, the body recognizes it as something out of place. In an attempt to fix this 'problem,' cells called platelets rush to the site. They form a sort of plug, like a Band-Aid, and then attract more cells. This leads to a clot.
Stent Thrombosis: The Unwanted Guest
Stent thrombosis is a fancy term for when a blood clot forms specifically within the stent. It can block the artery completely, which isn't good news. In untreated cases, it can cause a heart attack or other serious problems. Timing is everything, with a higher risk usually within the first year.
Factors Influencing Clots
Several factors can increase the chance of clots forming in stents. Discontinuing antiplatelet medication, having uncontrolled diabetes, or smoking can up your risk. The body's reaction can vary, too, based on genetics and overall health.
| Risk Factor | Influence on Clot Formation |
|---|---|
| Stopping Blood Thinners | Higher risk of clot formation |
| Diabetes | Increases clotting tendency |
| Smoking | Quitting decreases risk significantly |
The key takeaway? Talk to your doctor about your specific risks and stick to the treatment plan. Preventing a blood clot can often be just a matter of being diligent with meds and lifestyle changes.
Balancing Risks and Benefits
Deciding to go for a drug-eluting stent isn't just about slapping a band-aid on a problem. It's about weighing the benefits against the potential for blood clots lurking in the shadows. So, how do you make those tricky decisions?
Understanding Advantages
These stents are pioneering in the world of coronary artery disease treatment. By slowly releasing medication, they keep arteries open and lower the chances of needing another procedure. That sounds impressive, right? For many folks with recurrent arterial narrowing, the benefits can dramatically improve life quality.
Calculating the Risks
However, the risk of clotting isn't something to ignore. The likelihood of blood clots forming can vary based on individual health factors, like diabetes or previous clotting issues. Not to mention the responsibility that comes with taking medications as prescribed—sometimes for an extended period. Miss a pill, and you might increase those risks.
Personalized Decision Making
When it comes to stents, one size doesn't fit all. A solid conversation with your healthcare provider can spell out the personal pros and cons. For instance, if you have a history of bleeding problems, your doctor might consider other options, or at least discuss how to manage them better.
Let's look at a quick snapshot of the risk-benefit scenario:
| Factor | Risks | Benefits |
|---|---|---|
| Medication Compliance | Non-compliance increases clot risk | Following the regimen reduces arterial blockage |
| Existing Health Conditions | Conditions like diabetes may increase risks | Can still prevent heart attacks derived from arterial issues |
Choosing to have a drug-eluting stent isn't black and white. It's about understanding your unique health scenario and making informed choices with a healthcare team you trust.
Practical Tips and Prevention Strategies
Dealing with blood clots in drug-eluting stents can be nerve-wracking, but there are practical steps you can take to minimize the risks. Here, we dive into some useful tips and strategies that can come in handy.
Stay on Top of Medications
First and foremost, don't skip your meds! Your doctor might prescribe blood thinners to keep those pesky clots at bay. Compliance really makes a difference. Missing doses can increase the risk of clotting right when you want to avoid it the most.
Regular Check-ups Are Vital
Don't underestimate the power of follow-up visits. Regular check-ups with your healthcare provider can ensure everything is running smoothly and that your stent is doing its job without causing trouble. They can also track the progress and adjust medications if needed.
Adopt a Heart-Friendly Lifestyle
Leading a healthy life helps more than you realize. Here’s a simple guide:
- Diet: Aim for a balanced diet rich in fruits, veggies, and whole grains. Ditch the high-fat and processed foods.
- Exercise: Keep moving! Regular physical activity can work wonders. Even a brisk walk helps to keep your blood flowing smoothly.
- Quit Smoking: We all know it’s harmful. It’s especially risky when you have a stent.
Beware of Symptoms
If you experience chest pain, shortness of breath, or any symptoms that feel off, don’t just brush it off. Seek medical attention. Acting quickly can prevent serious complications.
Use of Data and Monitoring
It's amazing how far technology has come. Nowadays, you can use apps and wearables to monitor your heart health, which can alert you of any odd changes or help track your medication schedules. Here's a quick look at how tech can assist:
| Technology | Benefit |
|---|---|
| Wearables | Track heart rate and warn you of irregularities. |
| Medication Apps | Remind you to take your medication on time. |
At the end of the day, keeping blood clots at bay is a team effort involving you, your doctor, and sometimes a bit of technology. These steps, while simple, offer great peace of mind and control over your health.


Jesse Weinberger
March 22, 2025 AT 01:27Emilie Bronsard
March 22, 2025 AT 21:55John Bob
March 23, 2025 AT 10:58Alex Grizzell
March 24, 2025 AT 03:22George Johnson
March 25, 2025 AT 02:56Rodrigo Ferguson
March 25, 2025 AT 10:08Mickey Murray
March 26, 2025 AT 00:25Kevin McAllister
March 26, 2025 AT 04:23Marcia Martins
March 26, 2025 AT 08:42Robert Bowser
March 26, 2025 AT 15:30Sue M
March 27, 2025 AT 06:53Rachel Harrison
March 27, 2025 AT 12:50Tiffanie Doyle
March 27, 2025 AT 17:17james landon
March 28, 2025 AT 00:23Jenn Clark
March 28, 2025 AT 06:12L Walker
March 28, 2025 AT 22:01giri pranata
March 29, 2025 AT 07:40Stuart Rolland
March 30, 2025 AT 05:20Kent Anhari
March 30, 2025 AT 15:41Jesse Weinberger
March 31, 2025 AT 14:20