Wrong Dose: Risks, Real Cases, and How to Avoid Medication Mistakes
When you take a wrong dose, an amount of medication that’s too high, too low, or given at the wrong time. Also known as medication error, it’s one of the most common causes of preventable harm in healthcare. It doesn’t always mean taking too much—sometimes it’s taking too little, missing doses, or mixing pills you didn’t mean to combine. The result? Side effects that feel like a new illness, lab tests that lie, or worse—hospital visits you never saw coming.
Take biotin, a popular supplement often taken for hair and nails. Also known as vitamin B7, it’s generally safe—but at high doses, it can throw off thyroid and heart tests, leading doctors to miss real problems like a heart attack or thyroid cancer. Or consider benzodiazepines, medications used for anxiety and sleep. Also known as benzos, they’re fine at the right dose—but in pregnancy, even slightly too much can raise the risk of birth defects, especially with drugs like alprazolam. These aren’t hypotheticals. Real people have been misdiagnosed, delayed treatment, or hospitalized because of a simple dosing mistake.
Furosemide, a diuretic used for fluid retention and high blood pressure. Also known as Lasix, it’s powerful—but if the dose is off, you can lose too much fluid, crash your blood pressure, or damage your kidneys. Same goes for opioids, painkillers like oxycodone or hydrocodone. Also known as narcotics, they’re effective when used right, but tapering too fast can trigger withdrawal, while taking too much can stop your breathing. Even something as simple as forgetting to skip a dose before a blood test can change your results. That’s why knowing your exact dose, why you’re taking it, and when to stop is just as important as knowing the name of the pill.
Most of these mistakes happen because people assume their doctor’s instructions are clear—or they’re too tired, stressed, or overwhelmed to double-check. Maybe you’re juggling multiple meds, or you’re helping an aging parent manage their pills. Maybe you’ve been on the same drug for years and stopped questioning the dose. But a small change—like switching from a 5mg tablet to a 10mg tablet without realizing it—can have big consequences.
The good news? You don’t have to guess. The posts below show real cases where wrong doses caused real problems—and how people fixed them. You’ll see how high-dose biotin fooled lab tests, how benzodiazepines in pregnancy need careful monitoring, how diuretics like furosemide can backfire if not timed right, and why opioid tapering must be slow and personalized. You’ll also learn what to ask your pharmacist, how to read pill labels correctly, and when to speak up if something feels off. This isn’t about fear. It’s about control. Because when it comes to your health, the right dose isn’t just a number—it’s your safety.
 18 Nov 2025
18 Nov 2025
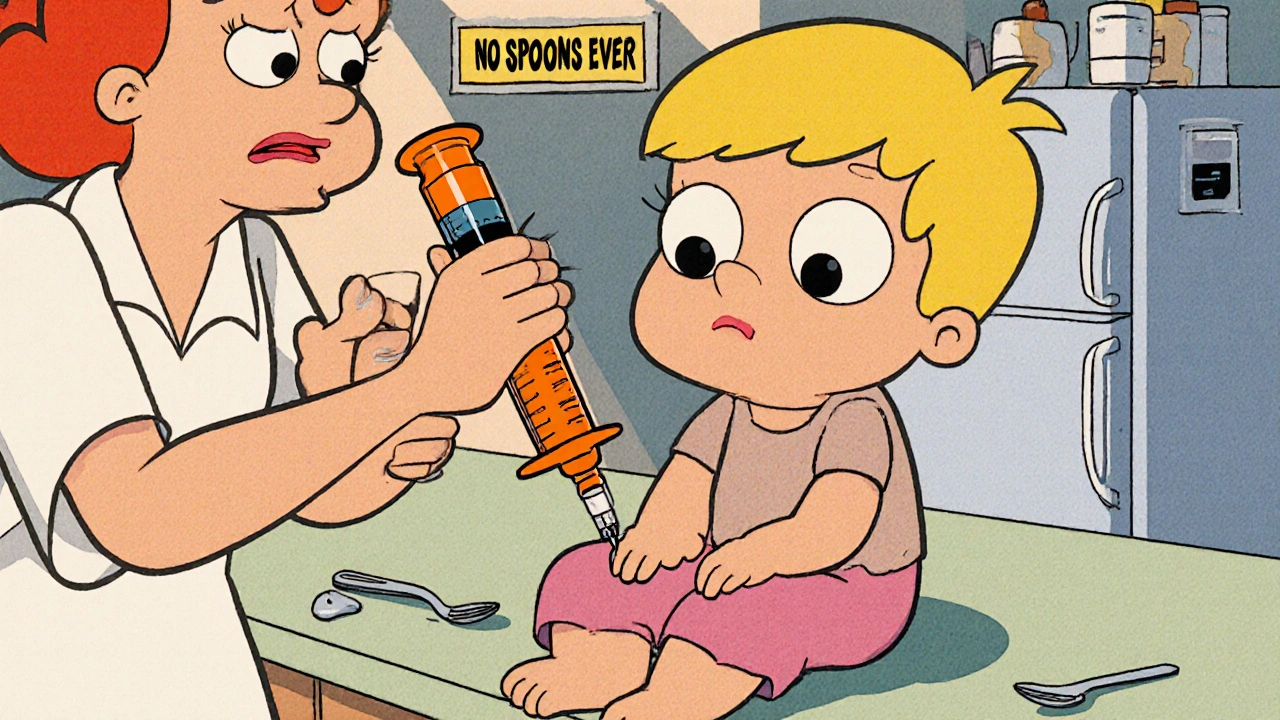
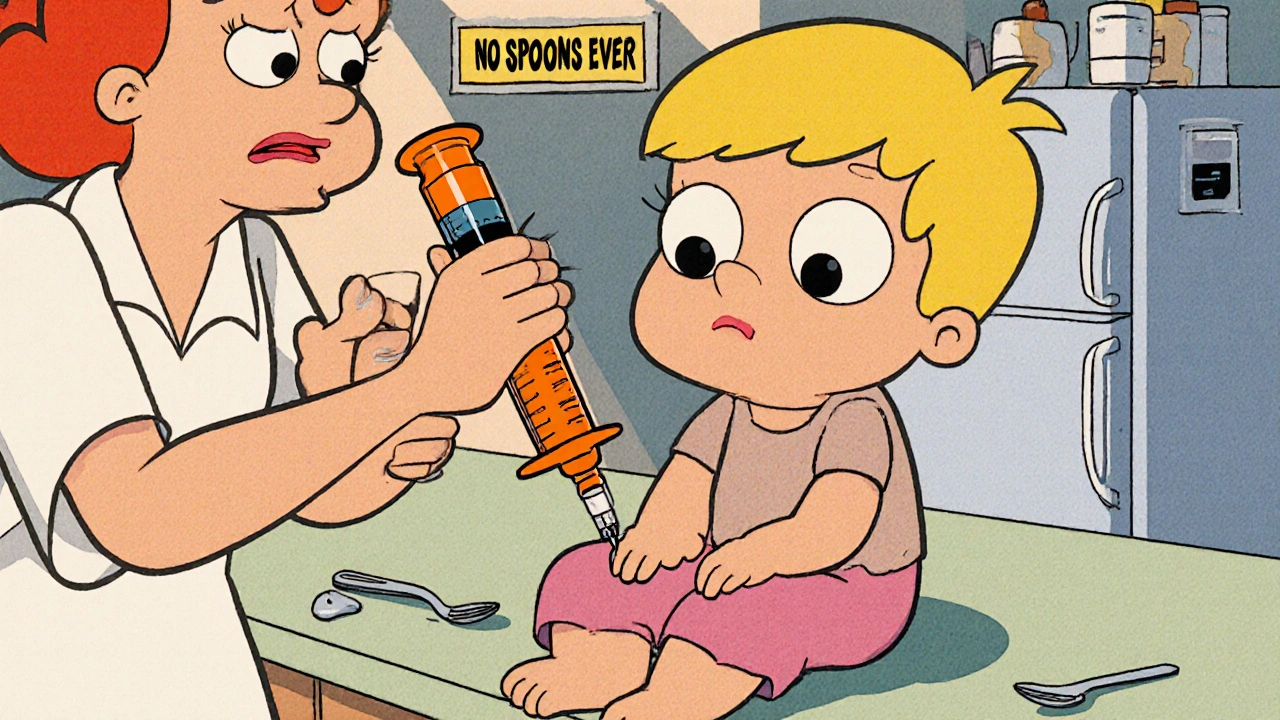
Learn how to prevent dangerous wrong-dose errors with liquid medications using oral syringes, metric measurements, and simple safety steps. Essential for caregivers and healthcare providers.
View More