Risk factors: how to spot what's putting your health at risk
Some risks you can change, and some you can’t. Knowing which is which makes a big difference. This page helps you quickly identify common risk factors, shows simple steps you can take right now, and explains when to talk to a doctor — especially if you’re starting or switching medications.
What counts as a risk factor?
A risk factor is anything that raises the chance of getting a disease or having a complication. Non‑modifiable risks include age, sex, and family history. Modifiable risks are things you can change: high blood pressure, high blood sugar, smoking, excess weight, poor sleep, low activity, bad diet, and risky drinking. Some risks come from medicines — drug interactions, side effects, or stopping a drug too fast.
Look at examples you might already know: uncontrolled blood pressure raises the chance of stroke and heart attack. Long‑term high blood sugar leads to nerve and kidney damage. Smoking increases the risk of heart disease, lung disease, and some drug complications. Recognizing the specific risk linked to a condition makes prevention practical, not vague.
How to check your personal risks
Start with a quick checklist: family history of heart disease or diabetes, your blood pressure, fasting blood sugar or A1c, cholesterol numbers, BMI or waist size, smoking status, alcohol use, daily activity, sleep quality, and current medications or supplements. Many clinics and pharmacies offer free blood pressure checks and basic screenings — use them. Keep a simple log for a few weeks: one page of readings and notes helps your doctor spot trends fast.
If you take prescription drugs, include that on the list. Some meds raise risk for falls, bleeding, or interactions with new prescriptions you might buy online. Before ordering medicine from a new pharmacy, check the label, confirm the exact drug and dose with your prescriber, and ask about interactions.
Small tests matter: a one‑time A1c or lipid panel can change your plan. If your blood pressure is consistently higher than 130/80, or fasting glucose is above normal, arrange a follow‑up. Don’t ignore repeated abnormal readings.
Quick signs to get help now: chest pain, sudden weakness or speech trouble, severe shortness of breath, new fainting, sudden severe headache, major bleeding, or signs of an allergic reaction. For medication side effects like confusion, sudden mood change, or severe dizziness, stop the drug only if your doctor tells you to — then seek urgent care.
Simple actions reduce a lot of risk: quit smoking, aim for 30 minutes of movement most days, cut added sugars and processed food, reduce alcohol, improve sleep, and follow your medication plan. Small wins add up: losing 5–10% of body weight, lowering salt intake, or starting a blood‑pressure medicine can change your outlook.
If you want reliable medication info or lower prices, use trusted pharmacy resources and confirm prescriptions with your clinician. Ask for a medication review if you take multiple drugs. That one conversation often prevents harmful interactions and lowers risk more than any single supplement.
Knowing your risks gives you control. Track key numbers, act on the modifiable ones, and check with a clinician when results change or symptoms appear. That’s how to turn risk into prevention.
 27 May 2023
27 May 2023
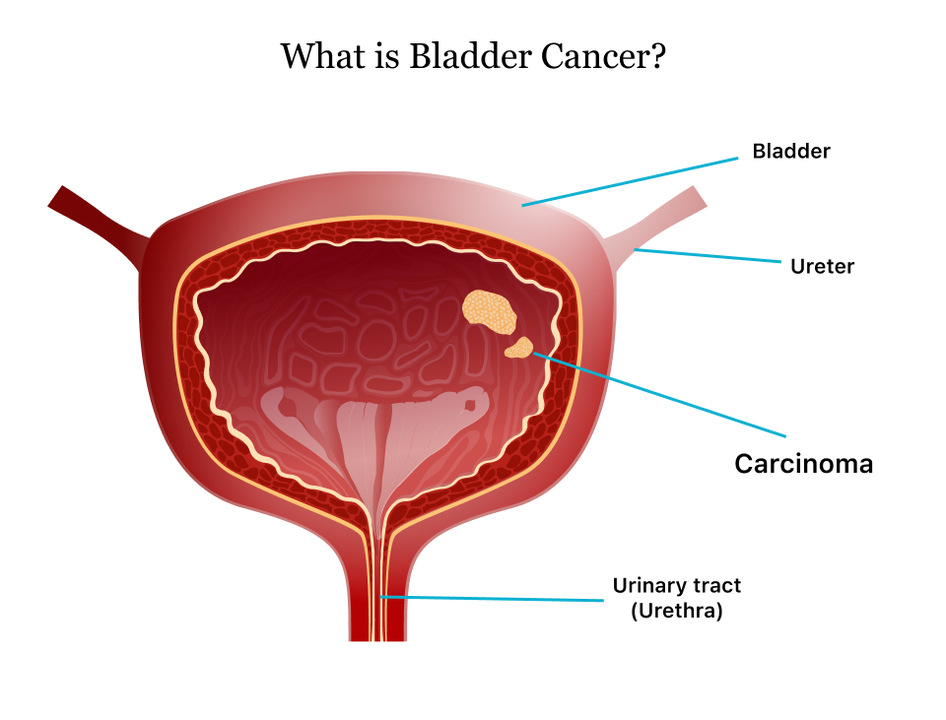
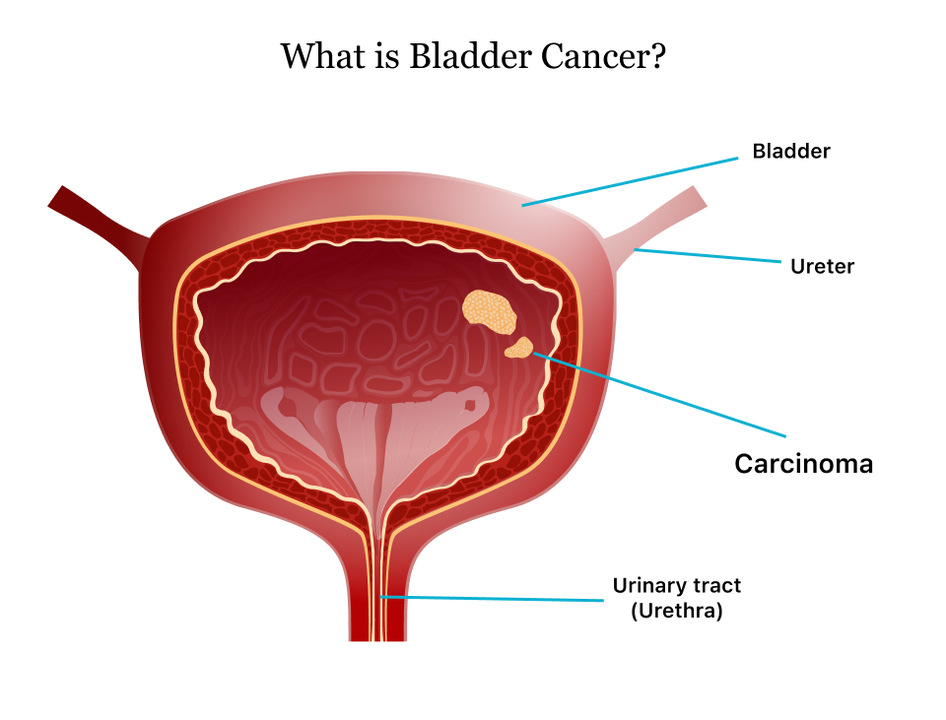
As a blogger, I've recently been researching the connection between urinary tract infections (UTIs) and bladder cancer. It's quite an eye-opening topic! From my findings, it appears that recurrent UTIs may increase the risk of developing bladder cancer, possibly due to the chronic inflammation caused by these infections. However, it's important to note that having a UTI doesn't mean you'll definitely get bladder cancer, but rather it's one of several potential risk factors. To better understand this connection, more research is needed, and in the meantime, it's crucial to seek prompt treatment for UTIs to maintain overall bladder health.
View More