Occupational Toxins: What You Need to Know
When working with occupational toxins, hazardous substances that workers may encounter on the job, ranging from chemicals to dust particles. Also known as workplace hazards, they can cause short‑term irritation or long‑term disease. Understanding these hazards helps you spot risks before they become a health problem.
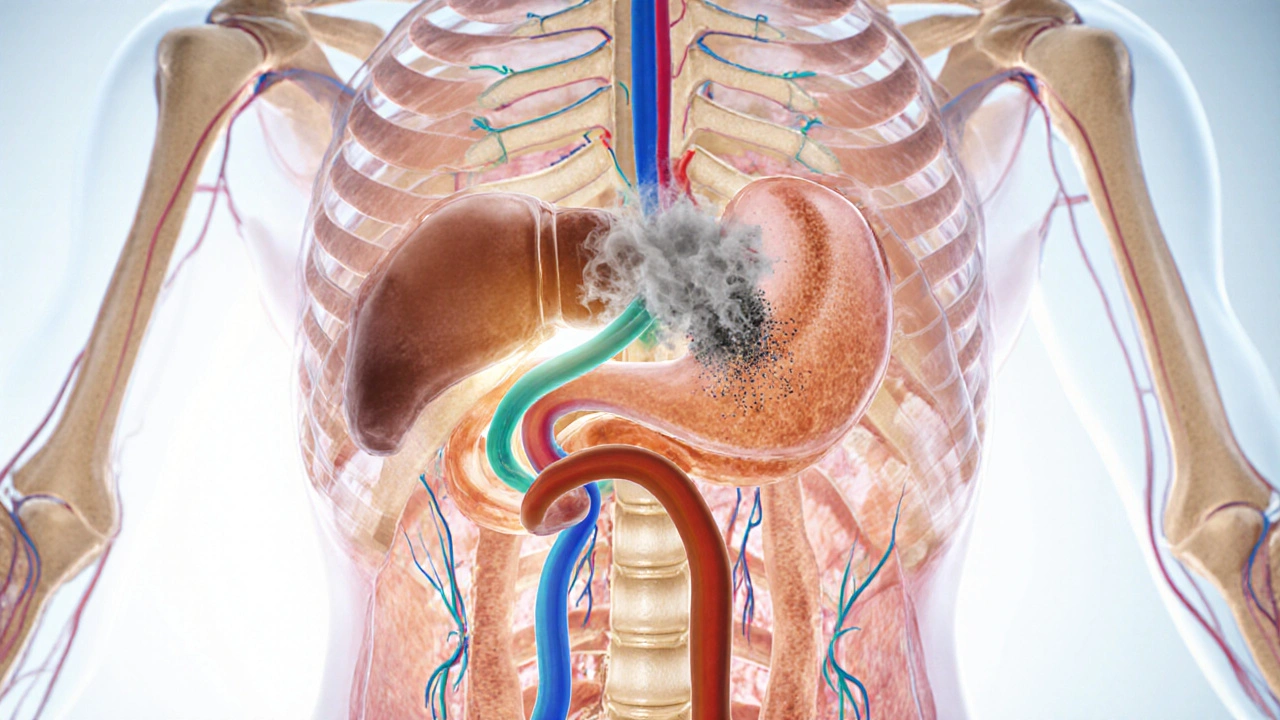
One of the most infamous examples is asbestos, fibrous mineral used in insulation and fire‑proofing that can lodge in the lungs. When inhaled, asbestos fibers trigger inflammation that may lead to mesothelioma or asbestosis. Another common culprit is lead, a heavy metal found in paint, batteries and some industrial processes. Lead exposure can impair cognition, cause anemia, and damage kidneys. Both agents illustrate how a single toxin can affect multiple organ systems.
Common Types of Occupational Toxins
Besides asbestos and lead, workers often encounter silica dust, tiny particles released during cutting, grinding or drilling of stone, concrete and sand. Repeated inhalation can cause silicosis, a progressive lung disease that reduces breathing capacity. Chemical solvents like benzene, toluene or xylene are also prevalent in painting, cleaning and manufacturing. These liquids dissolve fats and can be absorbed through the skin or lungs, leading to headaches, dizziness, and in severe cases, bone marrow suppression.
Occupational toxins don’t stay limited to the lungs. Some, like manganese dust, affect the nervous system, producing tremors and coordination problems. Others, such as formaldehyde, are known irritants that can trigger allergic reactions and increase cancer risk. The shared thread is that each toxin has a specific exposure route—air, skin contact, ingestion—so protecting workers means tackling each route with the right controls.
Regulatory agencies like OSHA and the WHO set exposure limits, but the numbers are only useful if they’re measured and enforced. Air‑monitoring devices, personal protective equipment (PPE) and regular health screenings create a safety net. For example, fit‑tested respirators filter out asbestos fibers and silica particles, while gloves and goggles shield skin from solvents and lead fumes.
Effective prevention starts with a risk assessment. Identify which processes generate toxins, quantify how much of each substance is present, and match that data with the appropriate control method. Substitution is the most powerful tool—replace a toxic solvent with a water‑based alternative if possible. If substitution isn’t feasible, engineering controls like ventilation hoods and enclosed workstations reduce airborne concentrations.
Training is another critical piece. Workers who understand how a toxin behaves are more likely to use PPE correctly and report unsafe conditions. Short, hands‑on sessions that explain the symptoms of lead poisoning or the early signs of silicosis keep safety top of mind.
Medical surveillance rounds out the program. Periodic blood tests for lead, lung function tests for silica exposure, and imaging for asbestos‑related disease catch problems early when they’re easier to treat. Early detection also provides data to refine workplace controls.
Technology is making monitoring easier. Wearable sensors now alert workers in real time when toxin levels exceed thresholds, prompting immediate action. Cloud‑based dashboards let managers see trends across multiple sites, enabling proactive interventions instead of reactive fixes.
When a toxin exposure does occur, prompt decontamination can limit damage. For skin contact, thorough washing with mild soap removes most chemicals. Inhalation incidents may require moving the worker to fresh air and administering oxygen if breathing is impaired. Having clear emergency protocols saves valuable minutes.
Finally, remember that occupational toxins don’t respect job titles. Construction crews, painters, welders, factory line workers, and even office staff handling old equipment can face hazardous substances. A universal safety culture that treats every employee as potentially exposed is the most resilient defense.
Below you’ll find a curated list of articles that dive deeper into specific toxins, compare treatment options, and offer step‑by‑step guides for safe purchasing of related medications. Whether you’re looking for practical tips on managing bladder issues in Parkinson’s or need a price‑check on generic antibiotics, the posts ahead cover a wide spectrum of health‑focused content that ties back to the risks and protections we’ve outlined here.