Environmental Risk Factor Calculator
This tool helps you understand how different environmental factors may contribute to your risk of developing chronic pancreatitis. Enter your information below to get personalized risk insights.
Risk Assessment Results
TL;DR
- Chronic pancreatitis is a progressive inflammatory disease that can be worsened by several environmental exposures.
- Heavy alcohol use, smoking, obesity, certain occupational chemicals, and air‑borne pollutants each raise risk, often by 1.5‑3times.
- Genetic susceptibility interacts with these factors, making some people especially vulnerable.
- Cutting alcohol, quitting smoking, maintaining a healthy weight, and limiting toxin exposure can slow disease progression.
- Clinicians should screen for environmental history and use a simple checklist to guide counseling.
What is chronic pancreatitis?
Chronic pancreatitis is a long‑lasting inflammation of the pancreas that gradually destroys tissue and impairs digestion. Over time the organ loses its ability to release digestive enzymes, leading to malabsorption, abdominal pain, and a higher chance of pancreatic cancer. The condition is irreversible, so understanding what drives it is crucial for prevention and early intervention.
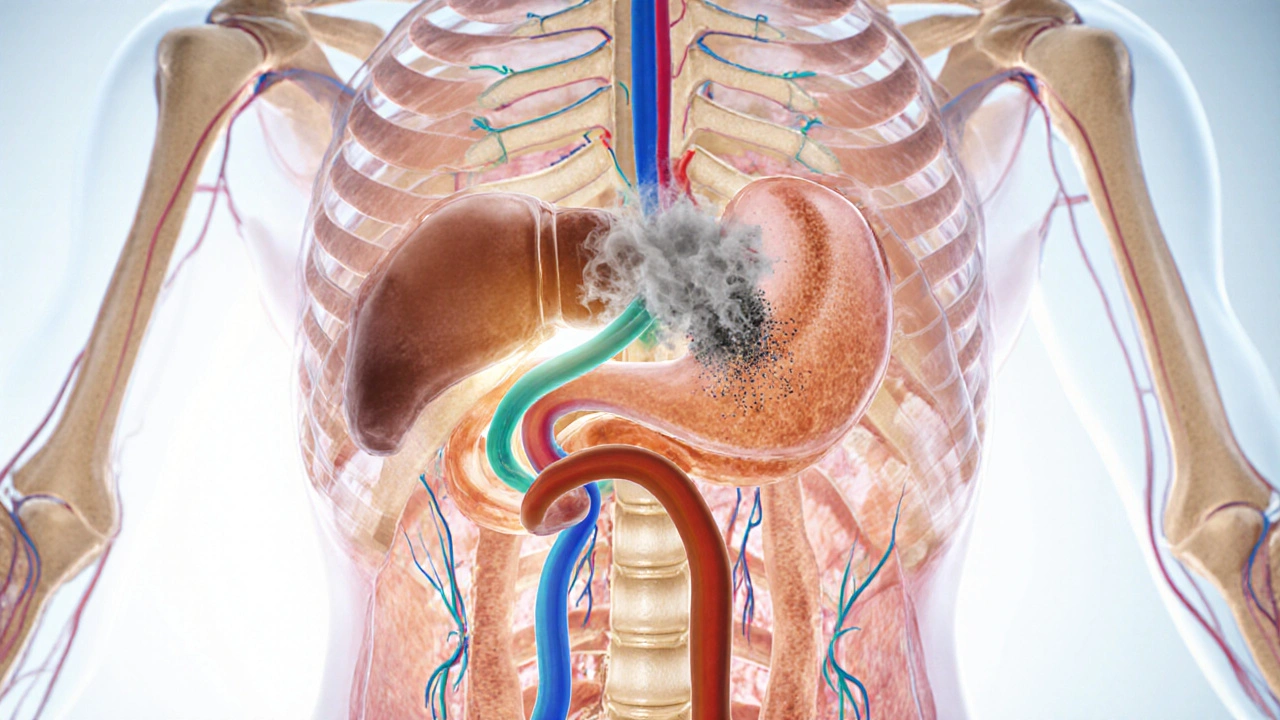
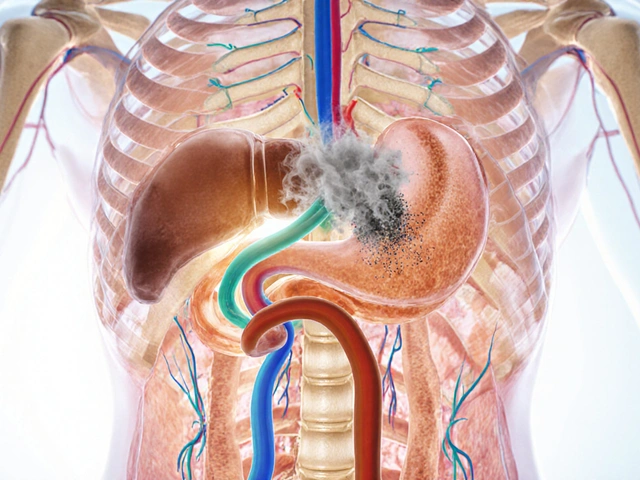
How do environmental factors reach the pancreas?
The pancreas sits deep behind the stomach, but it isn’t isolated. Blood vessels, nerves, and the duct system expose it to everything the body ingests or inhales. When a toxin circulates, it can accumulate in pancreatic tissue, trigger oxidative stress, or provoke an immune response that sparks inflammation. Think of the pancreas as a kitchen that can be polluted by the smoke from a neighboring grill; the longer the exposure, the more the equipment corrodes.
Major environmental risk factors
Below are the most consistently reported contributors.
Alcohol consumption is the single biggest modifiable risk factor for chronic pancreatitis worldwide
Studies from the US, Europe, and Asia show that drinking more than 40g of ethanol per day (roughly three standard drinks) raises the odds of developing chronic pancreatitis by 2‑4times. Alcohol directly damages pancreatic acinar cells, increases ductal viscosity, and promotes premature enzyme activation-essentially turning the organ’s own digestive juices against itself.
Smoking is an independent risk factor that compounds the harms of alcohol
Even in non‑drinkers, a habit of 20 cigarettes per day can boost risk by 1.5‑2times. Nicotine and tar generate free radicals that accelerate fibrosis (scar tissue formation) in the pancreas. When alcohol and smoking coexist, the risk can climb to more than sixfold.
Obesity and high‑fat diets are metabolic stressors that increase pancreatic inflammation
Body‑mass index (BMI) above 30kg/m² is linked with a 1.8‑fold higher incidence of chronic pancreatitis. Excess fat deposits around the pancreas release inflammatory cytokines, while high‑fat meals stimulate over‑production of digestive enzymes, setting the stage for premature activation.
Occupational exposure to chemicals such as organophosphates, heavy metals, and petrochemical solvents is associated with increased pancreatic injury
Workers in agriculture, mining, and manufacturing often inhale or absorb compounds that act as pancreatic toxins. A 2023 cohort of US pesticide applicators found a 2.2‑fold rise in chronic pancreatitis compared with non‑exposed peers.
Air pollution (PM2.5, nitrogen dioxide) is correlated with higher rates of pancreatic inflammation in urban populations
Fine particulate matter can travel through the bloodstream and lodge in pancreatic capillaries, provoking oxidative damage. Residents of cities with annual PM2.5 >35µg/m³ have a 1.4‑times greater risk than those in cleaner regions.
Pesticides and other agro‑chemicals are linked to pancreatic fibrosis through chronic low‑level exposure
In a pooled analysis of farming communities across Europe, cumulative exposure to organochlorine pesticides was tied to a 1.9‑fold increase in chronic pancreatitis diagnoses.

Interaction with genetics
Genetic variants-such as mutations in the PRSS1, SPINK1, and CFTR genes-already predispose individuals to pancreatic damage. When a genetically susceptible person also drinks heavily, smokes, or works with toxins, the disease can manifest decades earlier. This gene‑environment synergy explains why some patients develop chronic pancreatitis with modest alcohol intake while others tolerate higher levels without issue.
Prevention and lifestyle tweaks
Addressing environmental risk factors doesn’t require a complete life overhaul, but targeted changes make a measurable difference.
- Cut alcohol: Aim for ≤2 drinks per day for men, ≤1 for women. If you already have pancreatitis, abstinence is the safest route.
- Quit smoking: Nicotine replacement, counseling, or prescription meds raise quit rates by 30% compared with willpower alone.
- Manage weight: Losing 5‑10% of body weight can lower inflammatory markers and reduce pancreatic fat.
- Reduce toxin exposure: Use protective gear at work, ensure proper ventilation, and choose organic produce when possible.
- Monitor air quality: On high‑pollution days, stay indoors and use HEPA filters; consider a portable air purifier.
Quick clinician checklist
- Ask about alcohol quantity, frequency, and binge episodes.
- Document smoking history in pack‑years.
- Record BMI and dietary patterns (fat intake, processed foods).
- Inquire about occupational chemicals, pesticide use, and protective measures.
- Assess residential air‑quality data (use local AQI dashboards).
- Screen for family history of pancreatic disease and known genetic mutations.
- Provide tailored counseling based on the highest‑risk factors identified.
Comparison of key environmental risk factors
| Factor | Typical Exposure | Relative Risk (RR) | Primary Mechanism |
|---|---|---|---|
| Alcohol | >40g/day | 2‑4× | Acinar cell toxicity, ductal obstruction |
| Smoking | ≥20 cigarettes/day | 1.5‑2× | Oxidative stress, fibrosis |
| Obesity (BMI>30) | High‑fat diet, sedentary lifestyle | 1.8‑2× | Cytokine release, enzyme overload |
| Occupational toxins | Organophosphates, solvents, heavy metals | ~2× | Direct cellular injury, chronic inflammation |
| Air pollution (PM2.5>35µg/m³) | Urban residential exposure | 1.4‑1.6× | Systemic oxidative damage |
| Pesticides (cumulative) | Farm work, contaminated food | 1.9‑2× | Low‑level chronic toxicity |
Next steps for patients and providers
If you suspect environmental triggers are contributing to chronic pancreatitis, start with a detailed exposure history. Use the checklist above, then prioritize the highest‑risk habit for change. For most patients, quitting alcohol and smoking delivers the biggest health gain within weeks.
Healthcare providers should consider ordering baseline pancreatic enzyme tests and imaging when risk factors accumulate, especially if the patient reports persistent abdominal pain or weight loss. Early detection of exocrine insufficiency allows timely enzyme replacement, reducing malnutrition and improving quality of life.
Finally, keep an eye on emerging research. New biomarkers-such as serum trypsinogen‑2 and advanced imaging techniques-are being validated to catch pancreatic inflammation earlier in high‑risk populations.

Frequently Asked Questions
Can occasional drinking cause chronic pancreatitis?
Only when occasional binge episodes push daily ethanol intake above the 40g threshold does the risk rise noticeably. For most people, moderate consumption (<1 drink/day) carries a low risk, but if you have a genetic predisposition, even modest drinking may matter.
Is secondhand smoke a concern for pancreatic health?
Yes. Long‑term exposure to secondhand smoke has been linked to a 1.2‑1.3× increase in chronic pancreatitis risk, especially in combination with other factors like alcohol.
Do air purifiers actually lower pancreatic disease risk?
Air purifiers that filter fine particles (<0.3µm) can reduce indoor PM2.5 levels by up to 60%. While direct evidence on pancreas outcomes is limited, lowering systemic inflammation should theoretically reduce risk.
Should I get genetic testing if I have a family history of pancreatitis?
Testing for PRSS1, SPINK1, and CFTR mutations is advisable when multiple close relatives are affected or when disease appears at a young age. Knowing your genetic status helps tailor lifestyle advice.
Is there any medication that can reverse environmental damage to the pancreas?
No drug can fully reverse established fibrosis, but antioxidant supplements (e.g., vitaminE, selenium) and anti‑inflammatory agents may slow progression. The cornerstone remains removing the offending exposure.
Understanding the link between environmental factors chronic pancreatitis empowers both patients and clinicians to act before irreversible damage sets in. By cleaning up lifestyle choices and reducing toxin exposure, we can blunt the disease’s advance and improve everyday wellbeing.

Rod Maine
October 2, 2025 AT 22:06Honestly, this whole calculator feels like a pretentious attempt to make laypeople think they're scientists. The interface, while sleek, pretends to solve a problem that would be better addressed by a good ol' doctor asking you about your lifestyle, not a glorified spreadsheet. It’s clever, but the illusion of empowerment is a bit overhyped, y’know?
Othilie Kaestner
October 3, 2025 AT 20:20Well, I guess the American way is to blame everything on “environment.” Sure, smoking’s bad, but it’s the government’s job, not yours! Let’s not forget that foreign diets are the real culprits-our "freedom" to eat fast food is what’s killing us, not personal responsibility.
Sebastian Samuel
October 4, 2025 AT 15:46Wow, this tool is sooo informative 😍! I’m already feeling the weight of my habits, and it’s kinda terrifying 😱. If you’re reading this, just know you’re not alone-my anxiety spikes every time I think about my exposure levels 😔.
Mitchell Awisus
October 5, 2025 AT 16:46Interesting read; the data seems solid!; however, I think we could also discuss how socioeconomic status influences exposure-people in lower‑income neighborhoods often face higher air‑pollution levels; that’s a major oversight in many studies. Overall, good job highlighting the multifactorial nature of chronic pancreatitis.
Annette Smith
October 6, 2025 AT 09:26When we think about health, we must see the whole picture, not just one piece. The body works as a system, and each risk factor nudges it toward disease. Simple changes can shift the balance.
beth shell
October 7, 2025 AT 18:46Every small step matters. It’s about choosing water over soda, a walk over a drive. Consistency beats intensity.
khushali kothari
October 8, 2025 AT 08:40From a mechanistic standpoint, chronic exposure to organophosphates induces oxidative stress pathways, culminating in pancreatic acinar cell apoptosis. The cumulative dose–response relationship underscores the necessity for occupational health surveillance in agrarian cohorts.
Brandon Smith
October 9, 2025 AT 15:13Let’s be perfectly clear: the moral responsibility lies with the individual first, and second with the institutions that enable such harmful behaviors. While the calculator provides a veneer of scientific rigor, the underlying truth remains simple-people make choices, and those choices have consequences. Alcohol, smoking, and poor diet are not just “environmental factors”; they are personal decisions that reflect a lack of self‑discipline. If you plug in a daily intake of 50 grams of ethanol, you’ll see a high‑risk score, which is no surprise because the pancreas cannot tolerate that level of toxic exposure. The same logic applies to smoking: inhaling nicotine and tar delivers oxidants directly to the blood supply, which the pancreas then feels. The data supporting a 1.5‑to‑2‑fold increase in risk for heavy smokers is robust, derived from longitudinal cohort studies spanning decades. Obesity, measured as a BMI above 30, introduces excess adipose tissue, secreting inflammatory cytokines that exacerbate pancreatic inflammation. The synergistic effect-imagine a patient who drinks heavily, smokes a pack a day, and is obese-creates a perfect storm, amplifying the risk beyond the simple additive model. Occupational exposures to solvents and heavy metals further insult pancreatic ducts, and pesticide exposure in farming communities has been correlated with a nearly two‑fold increase in chronic pancreatitis diagnoses. The air‑pollution factor, though modest, still contributes systemic oxidative stress that cannot be ignored. When you consider genetics, such as PRSS1 or SPINK1 mutations, the environment acts as the catalyst that ignites the pathological cascade much earlier than it would otherwise occur. In practice, clinicians should prioritize lifestyle counseling: reducing alcohol intake to ≤2 drinks per day for men (≤1 for women), pursuing smoking cessation programs, and encouraging weight loss of 5‑10 % of body weight. Additionally, patients should be advised to use protective equipment at work, improve indoor air quality with HEPA filters, and opt for organic foods when possible to limit pesticide ingestion. Ultimately, the best defense against chronic pancreatitis is a proactive, holistic approach that marries personal responsibility with informed, evidence‑based recommendations. Remember: knowledge is only power when it translates into action.
darwin ambil
October 10, 2025 AT 13:26Okay, I get the info, but honestly, who has time to fill out all those fields? Just cut the booze and ditch the cigarettes, that’s the real fix. 😅
Kelvin Van der Maelen
October 12, 2025 AT 01:33Wow, another post about “risk factors.” I’m bored. Everyone knows smoking is bad; this is just rehashing old news. Can we get something fresh?
Joy Arnaiz
October 12, 2025 AT 21:00While the data may appear sound, one cannot ignore the possibility that pharmaceutical companies have a vested interest in inflating risk scores to promote drug sales. The narrative of environmental culpability conveniently shifts focus away from profit‑driven research agendas.
Christopher Eyer
October 14, 2025 AT 11:53Honestly this article is just a collection of generic statements with a few buzzwords. The author missed the bigger picture-there’s no mention of diet composition beyond BMI, which is a glaring oversight. Plus, the calculator feels like a gimmick rather than a real clinical tool.
Could have been better.
Mike Rosenstein
October 15, 2025 AT 15:40Great effort on pulling together multiple risk factors into a user‑friendly format. For clinicians, I’d suggest integrating this tool with electronic health records so that exposure data can be auto‑populated from patient questionnaires. That would streamline the workflow and improve accuracy.
Ada Xie
October 16, 2025 AT 23:36While the presentation is well‑structured, I note several typographical inconsistencies-e.g., “daily ethanol intake (grams):” versus “Cigarettes per day:” where the colon usage is irregular. Consistency in punctuation enhances readability.
Stephanie Cheney
October 18, 2025 AT 00:36Encouraging folks to take small, sustainable steps can really boost confidence. Even a modest reduction in alcohol or adding a short walk each day can shift the risk curve positively.
Georgia Kille
October 20, 2025 AT 08:10👍 Simple changes = big impact. Choose water, walk more.
Jeremy Schopper
October 22, 2025 AT 01:50Remember-consistent effort beats occasional intensity!; take one day at a time; celebrate each small victory; your pancreas will thank you!; stay motivated!