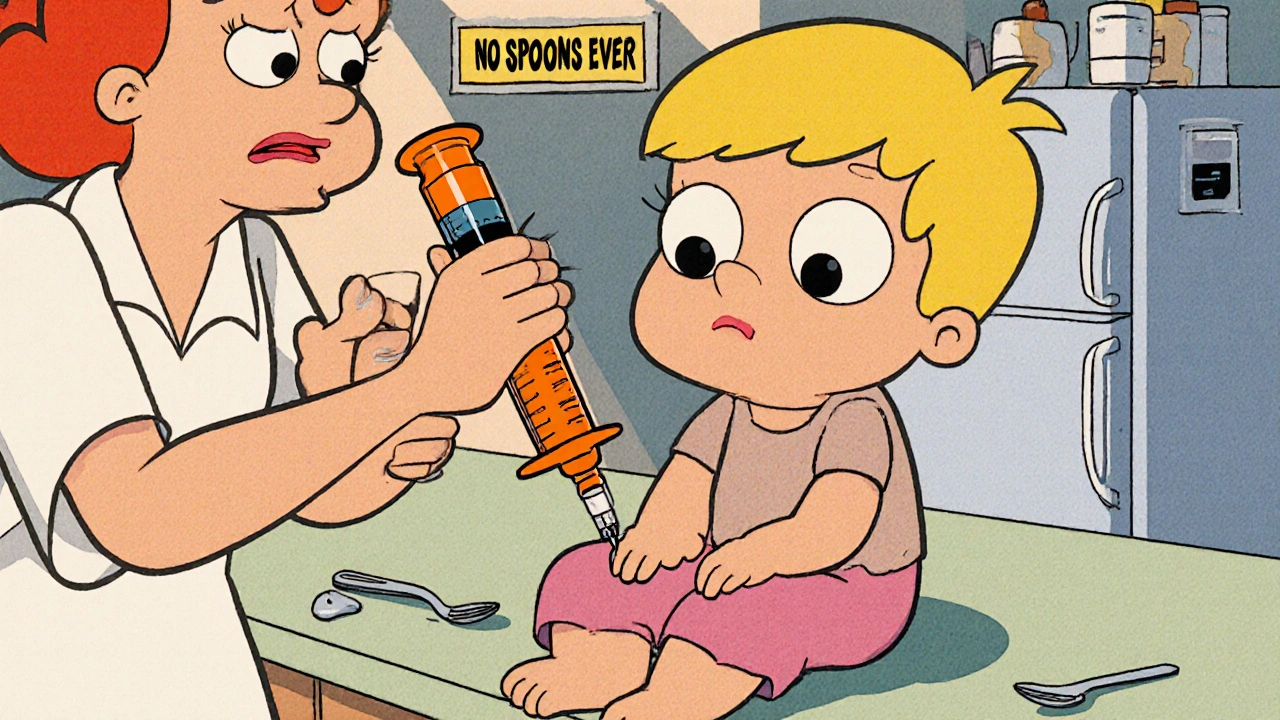
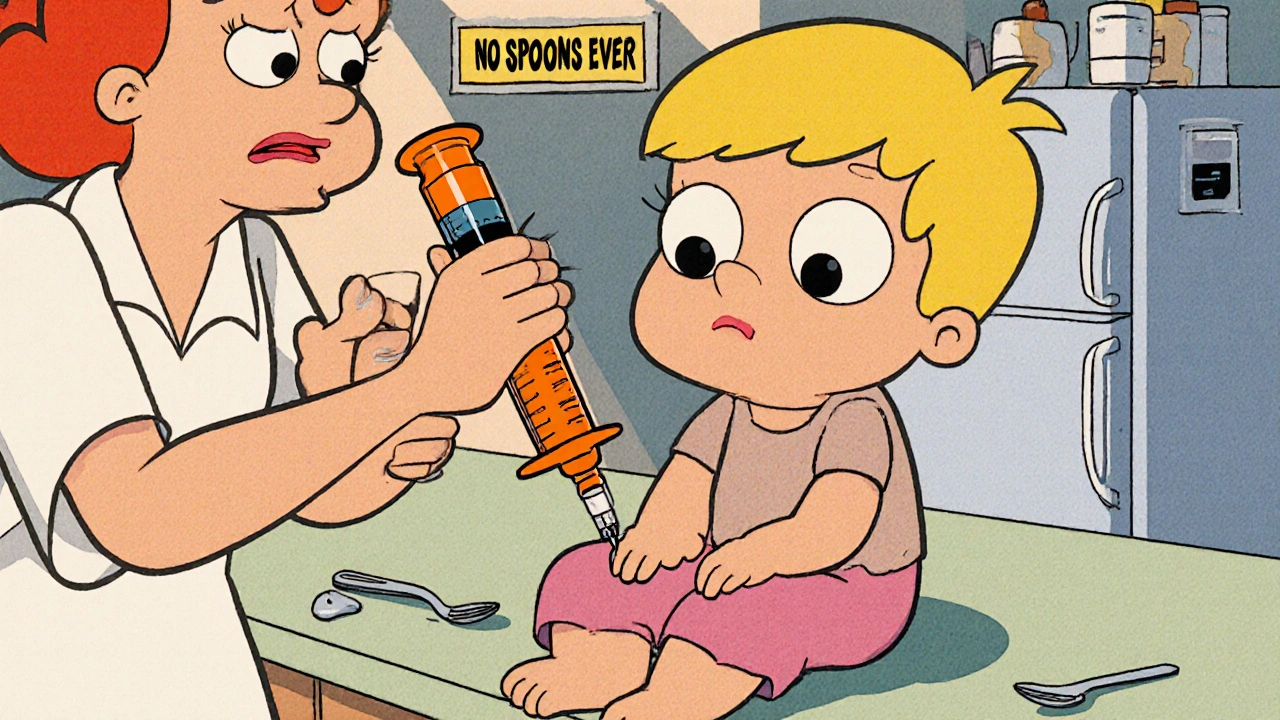
Liquid Medication Errors: How Mistakes Happen and How to Avoid Them
When you measure out liquid medication, a fluid form of a drug given by spoon, syringe, or cup, often used for children, elderly, or those who can’t swallow pills. Also known as oral liquid drugs, it’s meant to be precise—but small mistakes can have big consequences. A teaspoon isn’t a tablespoon. A syringe marked in milliliters isn’t the same as a kitchen spoon. These aren’t just technicalities—they’re the difference between healing and harm. The liquid medication errors you hear about in news reports? Most of them happen at home, not in hospitals. Parents give the wrong dose because they’re tired. Seniors mix up syringes because the labels are too small. Caregivers guess because the instructions are unclear.
These errors often involve pediatric dosing, the practice of calculating drug amounts for children based on weight or age, where even a 10% mistake can be dangerous. Furosemide, amoxicillin, or acetaminophen syrup might seem harmless, but too much can crash a child’s system. On the other end, medication safety, the set of practices designed to prevent harm from drugs, including accurate measurement, clear labeling, and patient education isn’t just a hospital policy—it’s something every family needs to understand. Studies show that over 40% of parents use kitchen spoons to give liquid meds, even though those spoons vary wildly in size. And if you’re giving a drug like dosing mistakes, incorrect amounts of medication due to misreading labels, confusing units, or using improper tools with a drug like benzodiazepines or opioids in liquid form, the risk goes up fast. These aren’t rare cases. They’re everyday problems hiding in plain sight.
It’s not just about the dose. It’s about the tool. A 5 mL oral syringe isn’t the same as a 10 mL one. A dropper labeled "for infants" might not match the concentration on the bottle. And don’t forget: some liquid meds come with different strengths—like 160 mg per 5 mL versus 80 mg per 5 mL. Mix those up, and you’re giving double the intended dose. Even the way you hold the syringe matters. Tilt it wrong, and you lose a drop. That drop could be the difference between control and crisis. That’s why drug administration errors, mistakes made when giving a drug to a patient, including wrong route, wrong dose, or wrong timing are so common. They’re not always about carelessness. Sometimes, they’re about confusion, fatigue, or bad design.
You don’t need to be a nurse to avoid these mistakes. You just need to be careful. Always use the syringe or cup that came with the medicine. Never guess. Write down the dose and time. Keep a log. Ask your pharmacist to show you how to measure it. If the label says "shake well," shake it. If it says "refrigerate," keep it cold. These steps aren’t optional—they’re your safety net. The posts below cover real cases where liquid meds went wrong, what went unnoticed, and how people fixed it. You’ll find guides on measuring tools, how to read labels clearly, what to do if you give the wrong dose, and how to talk to your doctor about safer options. This isn’t about fear. It’s about control. And you have more power than you think.
 18 Nov 2025
18 Nov 2025
Learn how to prevent dangerous wrong-dose errors with liquid medications using oral syringes, metric measurements, and simple safety steps. Essential for caregivers and healthcare providers.
View More