Bladder cancer — symptoms, tests, treatment, and what to ask your doctor
Bladder cancer often shows early signs you can notice: blood in your urine, a sudden need to urinate, or pain when peeing. These symptoms don't always mean cancer, but they deserve quick checks. Catching problems early gives you more treatment options and often better outcomes.
Risk factors are clear: smoking is the top one, followed by older age, certain workplace chemicals, chronic bladder inflammation, and previous pelvic radiation. Men get bladder cancer more often than women, but women tend to be diagnosed later. If any risk fits your history, mention it to your doctor.
What to expect at diagnosis
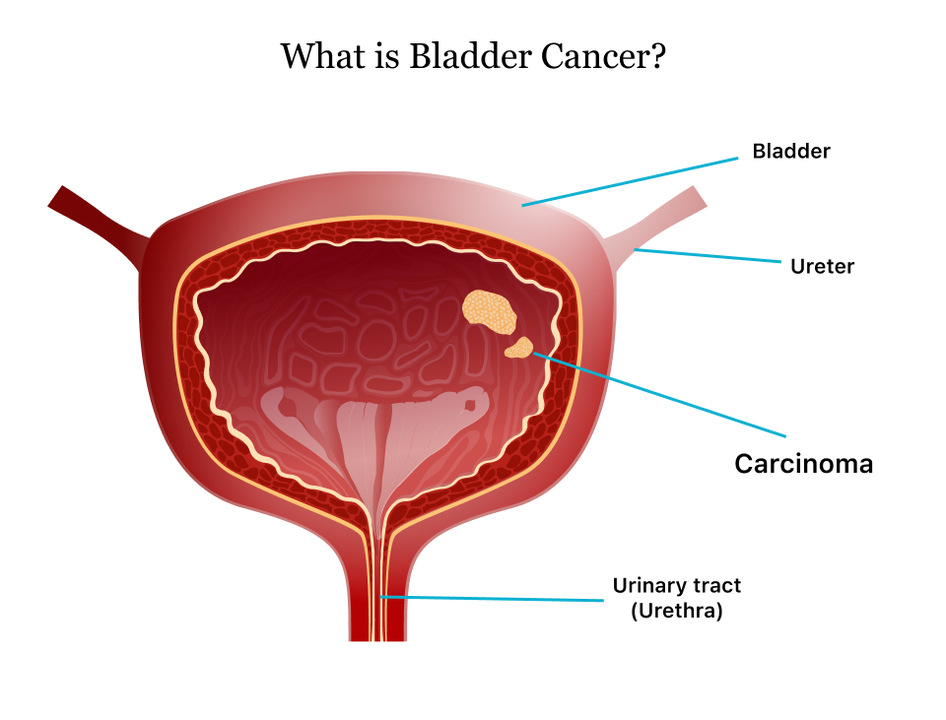
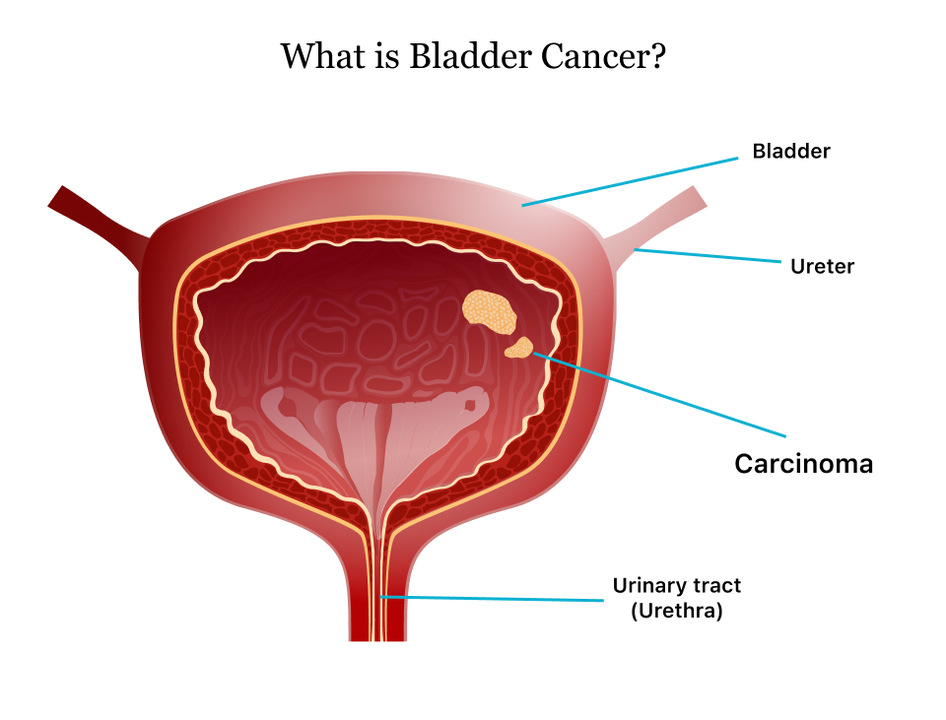
Your doctor will start with a urine test to look for blood and abnormal cells. If results are worrying, the next step is cystoscopy — a thin camera put into the bladder to look for tumors. Biopsy samples taken during cystoscopy confirm the diagnosis and tell whether the tumor is low-grade or high-grade. Imaging scans like CT or MRI check if the cancer has spread beyond the bladder.
Staging matters. Non‑muscle‑invasive tumors sit on the bladder lining and can often be removed with a scope, while muscle‑invasive cancers reach deeper tissue and need stronger treatment. Ask for clear staging language and what that stage means for your daily life and follow-up schedule.
Treatment options and everyday care
Treatment depends on stage and grade. Small superficial tumors may be removed with transurethral resection and followed with regular cystoscopies. More aggressive disease can need surgery to remove part or all of the bladder, chemotherapy before or after surgery, immunotherapy into the bladder, or systemic immunotherapy. Radiation is an option for some people.
Side effects vary. Bladder removal changes how you urinate and may require a urinary diversion or pouch. Chemotherapy and immunotherapy can cause fatigue, nausea, or immune reactions. Your care team should walk you through side effect management, diet tips, and when to call for problems like fever or severe pain.
Follow‑up is key. Bladder cancer often recurs, so expect frequent urine checks and cystoscopies in the first few years. Keep a simple symptom log—new bleeding, pain, or changes in urination—and bring it to appointments. Small notes help your doctor spot patterns fast.
Questions to ask: What is my exact stage and grade? What are the treatment goals—curative or control? What side effects should I expect and how are they managed? Will I need long‑term follow up and how often? Is there a clinical trial that fits my case?
BestPriceRx.com lists drug guides, safety tips, and cost-saving options for treatments used in bladder cancer care. Use those resources to compare medications and prepare for conversations with your medical team.
Lifestyle changes help recovery and reduce recurrence risk. Quit smoking, stay hydrated, and follow bladder-friendly habits like timed voiding and avoiding irritants (like strong perfumes and harsh soaps). Join a local or online support group to learn practical tips from others. Your oncologist or nurse can point you to reliable support and rehab services.
If you notice blood in urine or have risk factors, don’t delay. Early evaluation gives you choices and a clearer plan.
 27 May 2023
27 May 2023
As a blogger, I've recently been researching the connection between urinary tract infections (UTIs) and bladder cancer. It's quite an eye-opening topic! From my findings, it appears that recurrent UTIs may increase the risk of developing bladder cancer, possibly due to the chronic inflammation caused by these infections. However, it's important to note that having a UTI doesn't mean you'll definitely get bladder cancer, but rather it's one of several potential risk factors. To better understand this connection, more research is needed, and in the meantime, it's crucial to seek prompt treatment for UTIs to maintain overall bladder health.
View More