Most people think over-the-counter (OTC) drugs are safe because you don’t need a prescription. But that’s a dangerous assumption. Every year, millions of people - especially teens and young adults - take way more than the label says, not to feel better, but to get high. What starts as a one-time experiment can turn into a full-blown addiction, with serious health risks you might not even see coming.
What Does OTC Drug Misuse Actually Look Like?
It’s not just taking an extra pill. Misuse means using a medicine in a way it was never meant to be used. That could mean swallowing 10 cough syrup doses at once to chase a high, grinding up painkillers to snort, or taking loperamide (Imodium) by the handful to mimic opioid effects. The most common target? Dextromethorphan, or DXM, found in brands like Robitussin, Delsym, and Coricidin. At normal doses (15-30 mg), it’s a harmless cough suppressant. At 200-400 mg - that’s about 10-20 tablespoons of syrup - it starts to distort your senses. At 500 mg or more, you’re risking paralysis, hallucinations, and heart failure.
It’s not just DXM. Loperamide misuse has jumped 278% since 2011. People are taking up to 100 pills a day - 300 times the recommended dose - to get a high. The result? Heart rhythms go wild. QT intervals stretch past 500 milliseconds (normal is 350-440). That’s not just risky. It’s life-threatening.
Physical Signs You Can’t Ignore
These aren’t vague symptoms. They’re measurable red flags.
- Dilated or pinpoint pupils - seen in 78% of DXM abuse cases
- Slurred speech - articulation errors jump from 2% at normal doses to 68% when abused
- Unexplained weight loss - chronic users lose an average of 12.7 pounds in just three months
- High body temperature - reaching 103-105°F, sometimes leading to seizures
- Rapid heartbeat - heart rates spike from 70 bpm to 180 bpm
- High blood pressure - climbing from 120/80 to 160/100 or higher
- Liver damage - if the product contains acetaminophen (Tylenol), exceeding 4,000 mg a day can cause sudden, fatal liver failure
One Reddit user, ‘CoughSyrupSurvivor’, posted after a 1,200 mg DXM binge: “I couldn’t move for 8 hours. My heart was racing at 147 bpm. And the visual snow? It lasted three weeks.” That’s not a glitch. That’s brain chemistry being hijacked.
Behavioral Changes That Signal Trouble
Before the physical damage shows up, the behavior does.
- Sudden drop in grades - GPA plummets from 3.4 to 2.1 in one semester, according to Tennessee Department of Health data
- Secretive behavior - locking doors, changing phone passwords, hiding pills in vitamin bottles
- Unexplained spending - $127 a month vanishing without a trace, often on multiple brands of cough syrup
- Visiting multiple pharmacies - 87% of teens in one rehab study visited three or more pharmacies monthly to avoid detection
- Isolation - social interactions drop from 5.2 per day to 1.7
- Risky behavior - 3.2 times more likely to drive under the influence
These aren’t just “teenage mood swings.” They’re signs of a brain rewiring itself around a substance. The American Academy of Family Physicians found that 83% of teens abusing OTC meds pull away from friends and family - not because they’re “going through a phase,” but because they’re scared of being caught.
Psychological Damage Is Real - and Lasting
OTC drugs don’t just mess with your body. They mess with your mind.
- Mood swings - 5.7 times more frequent than in non-users
- Paranoia - episodes lasting 2-4 hours after the high wears off
- Emotional numbness - lasting 12-24 hours after use
- Persistent psychosis - 31% of chronic DXM users develop it, needing antipsychotic meds
- Memory loss - Dr. Nora Volkow of NIDA found an 8.3% reduction in hippocampal volume after six months of heavy DXM use
This isn’t temporary. The brain doesn’t bounce back easily. A 2023 study showed that even after stopping, many users still struggle with focus, memory, and emotional control - sometimes for years.
What Happens If You Don’t Stop?
The numbers don’t lie.
According to American Addiction Centers, 67% of people who start with OTC drug abuse move on to prescription pills or heroin within 18 months. Why? Because tolerance builds fast. Within 4-6 weeks, users need 3 to 5 times the original dose to feel anything. When cough syrup stops working, they turn to stronger stuff.
Emergency visits for OTC drug misuse have more than doubled since 2015 - from 6,200 to 14,700 in 2022. Each visit costs an average of $3,850. And that’s just the hospital bill. The real cost? Lost jobs, broken relationships, and irreversible brain damage.

What to Do If You or Someone You Know Is Misusing OTC Drugs
It’s not about shaming. It’s about acting.
Step 1: Don’t wait for a crisis. If you see three or more physical signs - say, slurred speech, dilated pupils, and elevated temperature - act immediately. Tennessee’s 2023 protocol shows 92% success in early intervention.
Step 2: Talk without judgment. Motivational interviewing - a calm, non-confrontational conversation - increases treatment engagement by 63% when done within 72 hours of noticing signs.
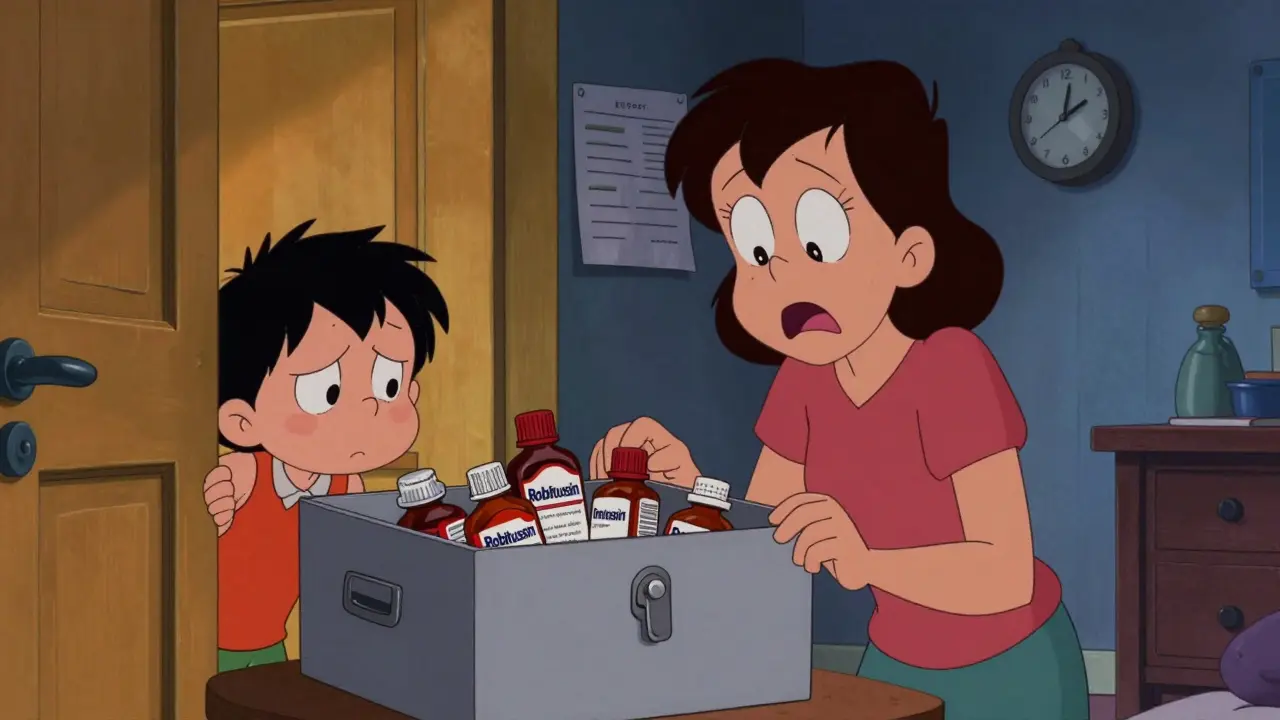
Step 3: Secure the meds. 72% of households keep OTC drugs in unlocked cabinets. That’s a recipe for disaster. Use a lockbox. Even a simple plastic box with a combination lock cuts misuse risk by 70%.
Step 4: Get professional help. Detoxing from DXM or loperamide isn’t like quitting caffeine. It requires medical supervision. Withdrawal can trigger depression, anxiety, and hallucinations. SAMHSA recommends 5-7 days of monitoring. Many need antidepressants afterward.
Step 5: Choose the right treatment. For teens, cognitive behavioral therapy + family therapy works best - 68% stay drug-free at six months. Individual therapy alone? Only 42%.
Prevention Is Possible - And It’s Working
Change is happening. Since 2021, 32 states have launched “Know the Dose” school programs. In 8th graders, first-time DXM misuse dropped 29%. The FDA now requires all DXM products to include a bold warning: “Taking more than directed may cause serious injury.” That simple change cut misuse by 14.3%.
There’s also new hope. The FDA approved the first loperamide-specific treatment in June 2023 - low-dose naltrexone - with 82% effectiveness in managing withdrawal. Researchers are testing a new drug to repair DXM-induced memory damage. Early results show 47% improvement after 12 weeks.
OTC drugs aren’t harmless. They’re powerful chemicals, and they’re easier to get than most people realize. But the good news? You don’t have to wait until it’s too late. Recognizing the signs early - the physical, the behavioral, the psychological - can change everything.
If you’re using these meds to escape, numb, or feel something - you’re not weak. You’re responding to pain. But you don’t have to do it alone. Help is out there. And it works.
Can you really get addicted to cough syrup?
Yes. Dextromethorphan (DXM) can cause physical dependence. After just 4-6 weeks of regular high-dose use, your body starts needing more to get the same effect. Withdrawal symptoms include anxiety, insomnia, cravings, and depression. Many people don’t realize they’re addicted until they try to stop and can’t.
Is it safe to mix OTC drugs with alcohol?
Absolutely not. Mixing DXM or loperamide with alcohol increases the risk of liver damage, respiratory depression, and sudden heart failure. Alcohol also makes hallucinations and loss of coordination worse. Emergency rooms see dozens of cases every month from this combo - and many end in ICU.
Why do teens abuse OTC drugs instead of illegal ones?
Because they’re easy to get, cheap, and don’t feel “illegal.” Many teens believe if it’s sold in a pharmacy, it’s safe. They don’t realize that taking 20 pills of cough syrup is the same as snorting a street drug - it’s just disguised as something ordinary.
How do I know if my child is hiding OTC drugs?
Look for empty boxes in the trash, bottles labeled as vitamins or supplements, or sudden changes in behavior - secrecy, mood swings, poor grades, or unexplained money missing. Many teens hide pills in sock drawers, behind books, or even in empty shampoo bottles. If you suspect misuse, check the medicine cabinet - and lock it if you haven’t already.
Can OTC drug abuse cause permanent brain damage?
Yes. Chronic high-dose DXM use has been linked to reduced brain volume in areas responsible for memory and emotion. Some users report lasting trouble with focus, decision-making, and emotional control - even after quitting. The brain can heal, but not always completely. Prevention is far better than recovery.
Where can I get help for OTC drug misuse?
Call SAMHSA’s National Helpline at 1-800-662-HELP (4357). It’s free, confidential, and available 24/7. They can connect you to local treatment centers, support groups, and counseling services. For teens, family-based therapy has the highest success rate. Don’t wait for a hospital visit to act - early help saves lives.



jay patel
February 1, 2026 AT 19:28man i read this and thought about my cousin who used to buy Robitussin in bulk from the gas station like it was candy
he said it made him feel like he was floating in a sea of neon lights
then one day he stopped answering texts for two weeks
turned out he was in the hospital with a heart rhythm so wild the nurses called it a disco beat
he’s clean now but says the visual snow still shows up when he’s tired
and yeah i know it’s just cough syrup but bro it’s not harmless
it’s like using a chainsaw to trim your hedges
Ansley Mayson
February 2, 2026 AT 01:10why are we acting like this is new
we’ve known for 20 years
parents just don’t care until their kid ends up in the ER
then they blame the pharmacy
not the kid
not the lack of supervision
not the fact they left the medicine cabinet unlocked like a damn open buffet
it’s not a crisis
it’s negligence
phara don
February 2, 2026 AT 11:23so if you take 100 imodium pills your QT interval goes past 500ms
wait so that’s like… 150ms above normal
is that really that bad
like i know it’s dangerous but is it worse than a beer and a Xanax combo
:|
Eli Kiseop
February 3, 2026 AT 17:22i used to do this in high school with my friend we’d mix dextromethorphan with soda and call it rocket fuel
we thought we were so smart
until one time i couldn’t move for 6 hours and my mom found me curled up in the bathroom
she didn’t yell
she just sat next to me and said i’m sorry you feel like you need this
that broke me more than any lecture ever could
now i’m two years clean
and i still get flashbacks of the visual snow
it’s not a trip
it’s a trap
Murarikar Satishwar
February 5, 2026 AT 10:05the statistics here are terrifying but also deeply human
the fact that 87% of teens visit three or more pharmacies monthly shows they’re not reckless-they’re resourceful in the wrong way
they’re trying to solve an emotional void with chemistry
and yes the brain damage is real but so is recovery
my brother took DXM for 11 months
lost 18 pounds
dropped out of college
but after 18 months of family therapy and a structured rehab program
he’s working as a peer counselor now
he says the hardest part wasn’t quitting
it was learning he deserved help
you’re not weak for needing it
you’re brave for asking
Marc Durocher
February 6, 2026 AT 16:15lol at the people who say "it’s just cough syrup"
you know what else is just cough syrup
your grandma’s medicine cabinet
your little brother’s backpack
the 200ml bottle you bought on impulse because it was on sale
and then suddenly you’re hallucinating your cat is talking in Klingon
and you’re wondering why your mom is crying
and why your heart feels like it’s trying to escape your chest
it’s not a party trick
it’s a slow-motion suicide
and nobody talks about it until it’s too late
larry keenan
February 6, 2026 AT 16:52the physiological mechanisms underlying dextromethorphan-induced neurotoxicity involve NMDA receptor antagonism and serotonin syndrome potential
the 8.3% hippocampal volume reduction observed correlates with functional impairment in episodic memory encoding
and the QT prolongation from loperamide abuse is dose-dependent and non-linear above 100mg daily
the clinical implications are significant
yet public health messaging remains under-resourced and emotionally reductive
we require targeted neuropharmacological education in secondary curricula
not just scare tactics
Akhona Myeki
February 7, 2026 AT 08:37in South Africa we have the same problem with codeine cough syrup
but at least here we call it what it is
addiction
not "experimenting"
not "teenage phase"
it’s a drug crisis disguised as a pharmacy aisle
and the government does nothing
while you all sit here debating whether 500mg is "too much"
my cousin died at 19 from liver failure from mixing it with cheap vodka
you don’t get a second chance
and your "it’s just cough syrup" attitude kills
Gary Mitts
February 8, 2026 AT 10:23lock the meds
talk early
don’t wait
you got this