When a life-saving drug runs out, who gets it? This isn’t science fiction. In 2023, more than 300 drugs were in short supply across the U.S., including critical cancer treatments like carboplatin and cisplatin. Hospitals faced impossible choices: give a dose to a patient with a 70% chance of survival, or hold it for someone with a 20% chance? These aren’t just clinical decisions-they’re ethical ones. And without clear rules, they’re made in silence, often by exhausted clinicians under pressure.
Why Medication Rationing Happens
Drug shortages aren’t random. They’re the result of broken supply chains, manufacturing failures, and a market that favors cheap generics over reliable production. Three companies control 80% of the generic injectable drug market. If one factory shuts down-because of contamination, labor issues, or regulatory delays-dozens of hospitals lose access to essential medicines. In 2023, the FDA recorded 319 active shortages. Oncology drugs made up nearly half of them. When carboplatin disappeared, 70% of U.S. cancer centers couldn’t treat patients as planned. No one planned for this. But someone had to decide who got treated.What Ethical Rationing Looks Like
Ethical rationing isn’t about picking favorites. It’s about using consistent, transparent rules to avoid chaos. The most respected framework comes from Daniels and Sabin: accountability for reasonableness. It demands four things:- Publicity: Everyone knows how decisions are made.
- Relevance: Decisions are based on medical evidence, not personal bias.
- Appeals: Patients and families can challenge a decision.
- Enforcement: There’s oversight to make sure rules are followed.
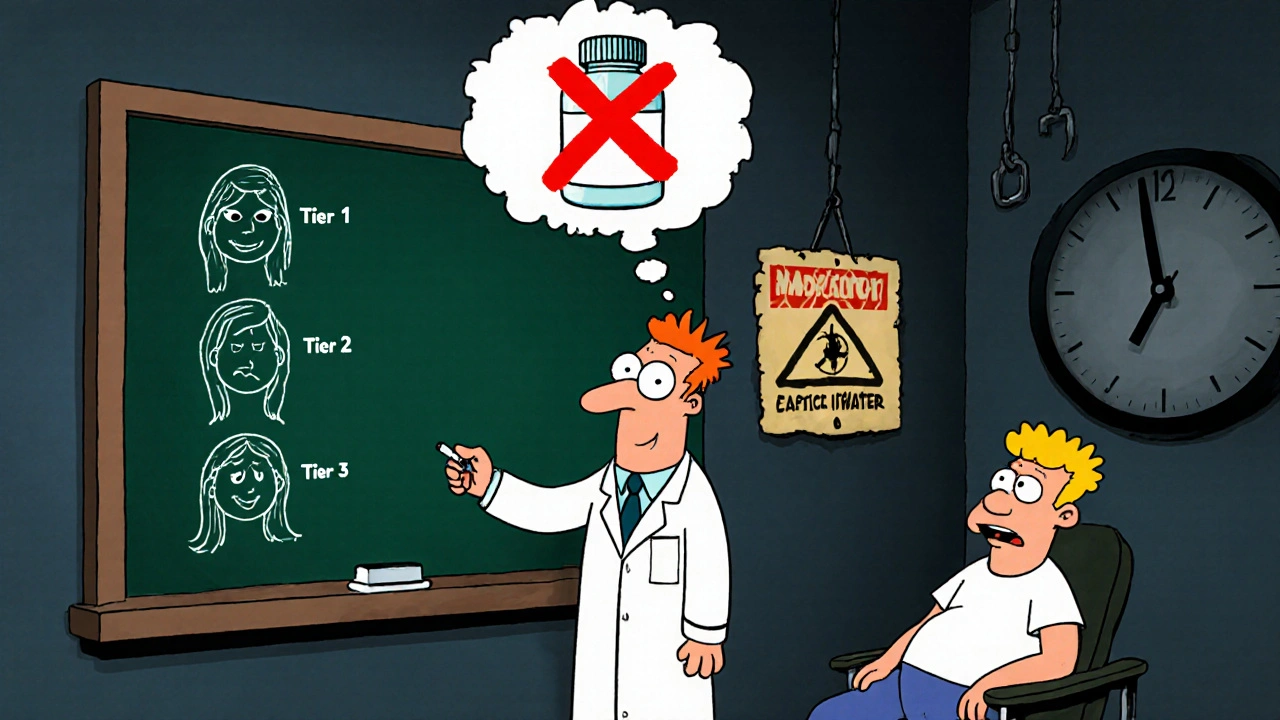
- Urgency: Is the patient’s condition life-threatening right now?
- Likelihood of benefit: Will this drug actually help?
- Duration of benefit: Will the patient live longer, or just get a few extra weeks?
- Years of life saved: Who stands to gain the most time?
- Instrumental value: Should a frontline nurse or firefighter get priority if they’re essential to saving others?
What Happens When There’s No System
Too often, there’s no committee. No rules. No transparency. In 2022, a study of 247 pharmacy managers found that over half of rationing decisions were made at the bedside-by one doctor, under pressure, without input. This leads to chaos. One patient gets a dose because their oncologist knows the pharmacist. Another doesn’t because they’re quiet, uninsured, or from a rural clinic. A 2022 JAMA study showed hospitals with formal committees had 32% fewer disparities in who got treated. Clinicians suffer too. When doctors are forced to choose who lives and who doesn’t without support, burnout spikes. One oncologist on ASCO’s forum said she had to choose between two stage IV ovarian cancer patients for limited carboplatin-three times in one month. No guidelines. No backup. Just guilt. And patients? Only 36% are told they’re being rationed. That’s not just unethical-it’s dangerous. When people don’t know why their treatment changed, trust in the system collapses.
Why Some Hospitals Still Don’t Have Rules
You’d think every hospital would have a plan. But only 36% had standing rationing committees as of 2018. Even fewer included ethicists-just 2.8%. Rural hospitals are hit hardest: 68% have no formal protocol. Why? It’s not laziness. It’s cost, complexity, and resistance. Setting up a committee takes time. The ASHP recommends at least 90 days of preparation: training staff, drafting policies, hiring ethicists, building communication tools. Many hospitals don’t have the staff or budget. Doctors often resist, saying, “I know my patient best.” But when every doctor thinks that, the system becomes a lottery. There’s also fear. Hospitals worry that if they admit rationing is happening, they’ll face lawsuits or bad press. But silence doesn’t protect them-it makes things worse. When patients find out later, they don’t blame the system. They blame the doctor. And the hospital.What Works: Real Examples
Hospitals that did it right saw results. At Mayo Clinic, after implementing a formal ethics committee model, clinician distress scores dropped 41%. At a large urban hospital in Chicago, they introduced a real-time EHR tracking system where every rationing decision had to include a justification and proof of patient communication. Within six months, complaints dropped by 58%. ASCO’s 2023 guidance pushed for a new standard: patients must be told. Not just informed-understood. They developed a script for doctors: “We’re running low on this drug. The rules say we give it to people who are most likely to benefit. Your case is being reviewed by our committee. We’ll let you know by tomorrow.” Simple. Honest. Human. Even small changes help. Some hospitals started using the lowest effective dose, stretching supplies further. Others switched to alternatives like nedaplatin when cisplatin wasn’t available. These aren’t perfect-but they’re better than nothing.
The Bigger Picture: Why This Keeps Happening
Rationing isn’t a temporary crisis. It’s a symptom of a broken system. The FDA projects drug shortages will keep rising-25% to 30% annually through 2027. Why? Because manufacturers have little incentive to make cheap generics reliably. It’s cheaper to shut down a plant than fix it. The 2012 law requiring manufacturers to notify the FDA of shortages? Only 68% follow it. The solution isn’t just better hospital policies. It’s national action. The FDA’s new AI-driven early warning system, launching in 2025, could predict shortages before they happen. The National Academy of Medicine is working on standardized ethical metrics-expected in early 2024. And the American Society for Bioethics and Humanities is launching certification for hospital committees in 15 states by January 2024. But none of this matters if hospitals wait until the drug is gone to act. Preparation is the only ethical choice.What You Can Do
If you’re a patient: Ask. If your treatment changes unexpectedly, ask why. Ask if there’s a rationing policy. Ask if you were considered in the decision. You have the right to know. If you’re a clinician: Push for a committee. Don’t wait for permission. Start the conversation with your pharmacy director, your ethics board, your hospital leadership. Bring the data. Bring the stories. Show them what happens when there’s no plan. If you’re a policymaker: Fund this. Require transparency. Penalize manufacturers who don’t report shortages. Make ethical allocation part of hospital accreditation.What’s Next
The next big step? Standardization. Right now, every hospital does it differently. One uses age. Another uses survival odds. Another uses insurance status-unintentionally. That’s not ethics. That’s inequality. The goal is simple: no patient should be left behind because of where they live, who they know, or how loud they are. The tools exist. The ethics are clear. What’s missing is the will to use them.Medication rationing shouldn’t be a secret. It shouldn’t be a burden on one doctor. It should be a system-fair, clear, and built on the idea that every life has value. Even when there’s not enough to go around.

Travis Freeman
November 30, 2025 AT 08:04Honestly, this is one of those topics that hits different when you’ve seen it up close. I had a cousin go through chemo during a shortage-got lucky, her oncologist had a connection. But knowing someone else didn’t? That’s the real tragedy. We need systems, not luck. Glad to see places like Mayo are making progress. Let’s scale this everywhere.
Sean Slevin
November 30, 2025 AT 14:46So… let me get this straight… we’re saying that if a drug is in short supply, we should… prioritize… people who are… most likely to benefit… based on… medical evidence… and… not… who… shouts loudest… or… who… knows… the pharmacist…? Wow. That’s… radical. Like… actual… ethics. Who… even… thought… of… that…?!!!
Chris Taylor
December 1, 2025 AT 04:46I work in a rural ER. We’ve had to skip antibiotics, insulin, even epinephrine. No committee. No guidelines. Just me, a phone call to the pharmacy, and a prayer. This article? It’s not theoretical. It’s Tuesday. We need help. Not just policies-funding, people, time. Someone’s gotta step up.
Melissa Michaels
December 2, 2025 AT 00:03The data presented here is compelling and aligns with existing bioethics literature. Formalized allocation protocols reduce clinical distress and mitigate inequities. The absence of ethicists in 97.2% of institutions is unacceptable. Hospitals must integrate ethics into operational planning-not as an afterthought, but as a foundational component of care delivery.
Nathan Brown
December 2, 2025 AT 15:10I get why people are scared to talk about this. But silence doesn’t protect anyone. It just makes the guilt heavier. I’ve sat with patients who asked, ‘Why didn’t I get it?’ and had no answer. No one told them. No one trained us to say it. We need scripts. We need permission. We need to stop pretending this isn’t happening. And yeah… I cried after my third rationing decision last month. I’m not proud of that. But I’m not alone.
Matthew Stanford
December 3, 2025 AT 07:25Good stuff. Let’s not forget: this isn’t just about drugs. It’s about who we are as a society. If we can’t decide who gets medicine fairly, how are we supposed to handle anything else? Start small. Talk to your hospital. Push for a committee. Even if it’s just 3 people. One voice can start a movement.
Olivia Currie
December 4, 2025 AT 11:23OH MY GOSH. I JUST CRIED READING THIS. 😭 This is the kind of thing that should be on the news every night. Not just for cancer patients-for EVERYONE. Diabetics. Asthma. Epilepsy. We’re living in a dystopia and no one’s talking about it! Someone call Netflix. This needs a documentary. NOW.
Curtis Ryan
December 4, 2025 AT 14:58so like… if we just… fixed the factories… and made sure the companies… didn’t… shut down… for no reason… we wouldn’t have this problem… right? like… why is this even a thing…? someone just needs to… fix it…
Rajiv Vyas
December 5, 2025 AT 19:25lol this is all just a psyop to get you to trust the government more. The real reason drugs are short? They’re being hoarded by the shadow pharmaceutical cartel to push you toward mRNA shots and biometric ID chips. You think they care if you live? Nah. They want you dependent. Read the 2018 Senate hearing transcript. It’s all there.
Astro Service
December 6, 2025 AT 02:28Why are we giving medicine to people who are sick? Why not give it to real Americans? Like soldiers or cops or teachers? Those people actually matter. This whole system is broken because we care more about some guy with cancer than the guy who protects the country. Wake up.
DENIS GOLD
December 6, 2025 AT 03:47Wow. So the solution to a broken supply chain… is… more committees? More paperwork? More bureaucrats? Brilliant. Next you’ll tell us we need a committee to decide who gets air to breathe. At this point, just let the market work. If you can’t afford it, don’t buy it. Simple.