Every year, tens of thousands of people end up in the hospital because of something many think is completely safe: an over-the-counter painkiller. NSAIDs like ibuprofen, naproxen, and aspirin are everywhere - in medicine cabinets, gym bags, and kitchen drawers. People take them for headaches, back pain, arthritis, or even after a long run. But for those with kidney disease or even just reduced kidney function, these drugs can trigger a sudden and dangerous drop in kidney function - acute kidney injury - often without warning.
How NSAIDs Hurt the Kidneys
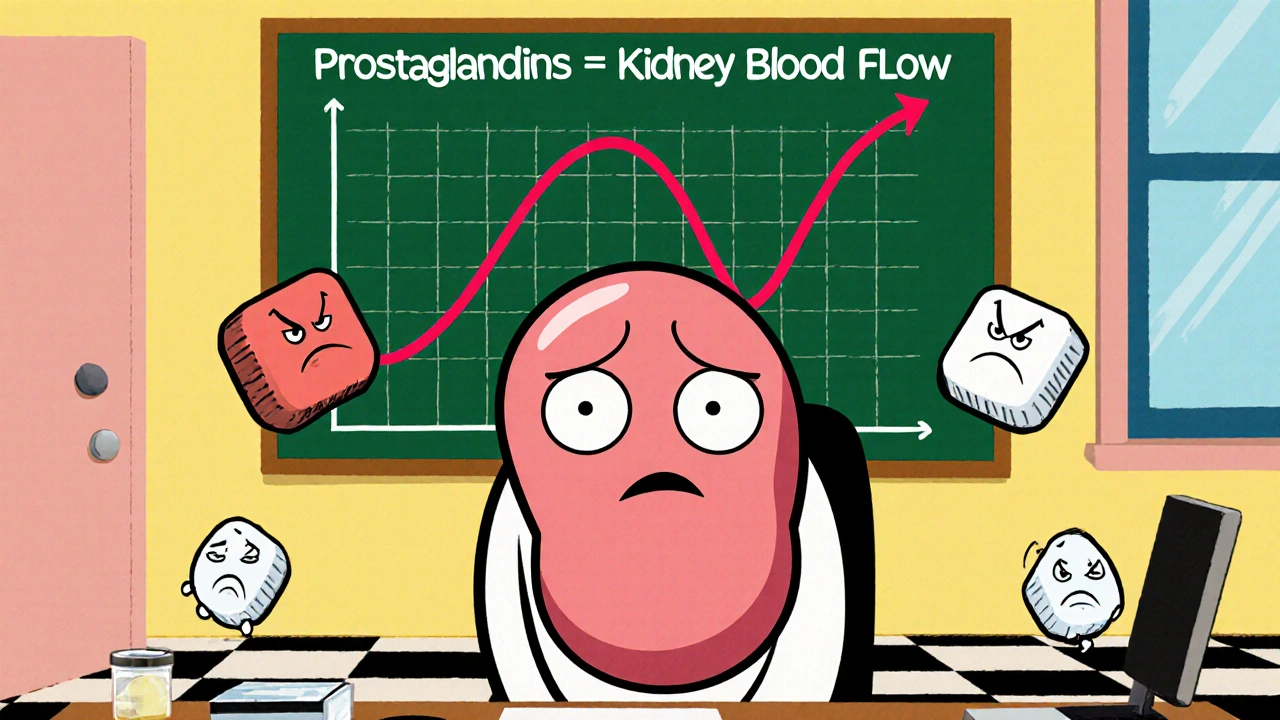
NSAIDs work by blocking enzymes called COX-1 and COX-2, which make prostaglandins. These tiny molecules aren’t just involved in pain and swelling - they’re critical for keeping blood flowing to your kidneys. When you take an NSAID, you reduce prostaglandin levels. That causes the tiny blood vessels in your kidneys to tighten. For a healthy person, this might not matter much. But if your kidneys are already working hard to compensate for something else - like dehydration, heart failure, or high blood pressure - this extra squeeze can cut off their blood supply.
This isn’t theoretical. Studies show that within 24 hours of taking an NSAID, someone with early kidney disease can see their glomerular filtration rate (GFR) drop by 20 to 40%. That’s like your kidneys suddenly losing nearly half their ability to filter waste. And because serum creatinine - the usual test doctors use to check kidney function - doesn’t always rise right away, many people don’t realize their kidneys are in trouble until it’s too late.
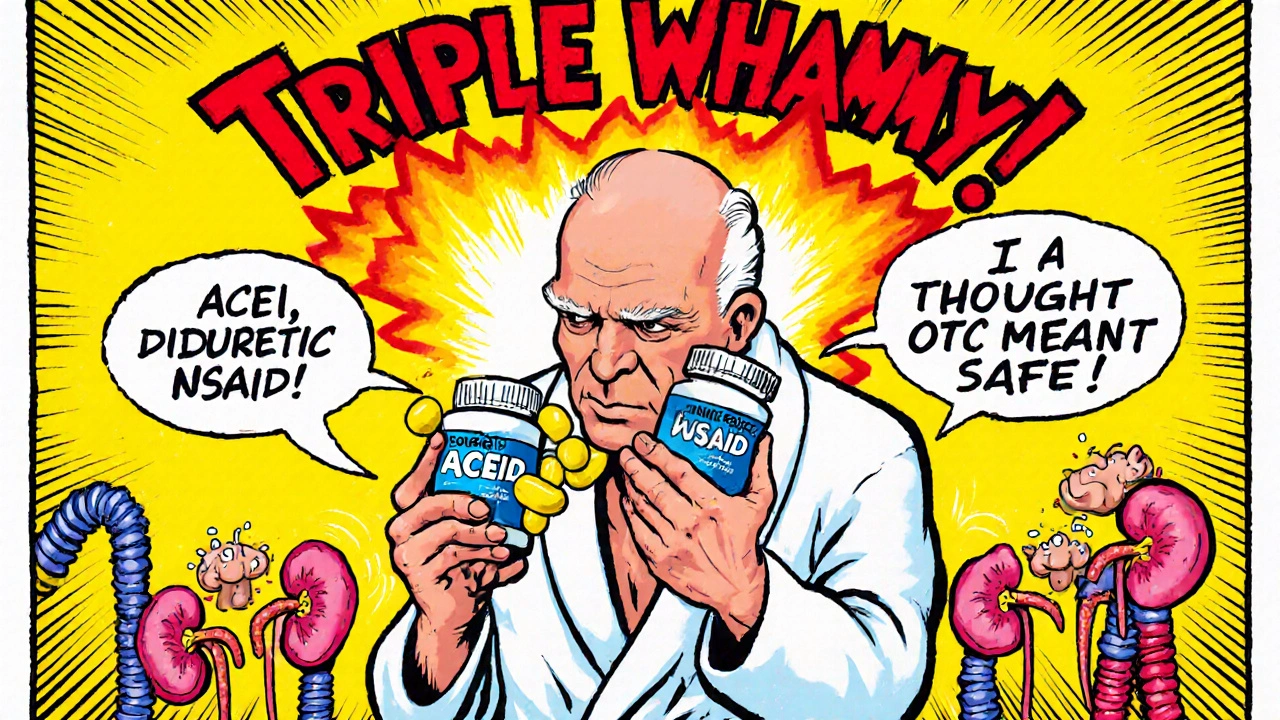
The Triple Whammy: When NSAIDs Combine With Other Drugs
One of the most dangerous situations happens when NSAIDs are taken with two other common medications: ACE inhibitors or ARBs (used for high blood pressure) and diuretics (water pills). Together, these three form what nephrologists call the “triple whammy.”
Here’s why it’s so risky:
- ACE inhibitors and ARBs relax blood vessels, which lowers blood pressure but also reduces kidney perfusion.
- Diuretics remove fluid from your body, which can lead to volume depletion.
- NSAIDs block the prostaglandins your kidneys need to compensate for both of those effects.
Research shows this combination increases the risk of acute kidney injury by 31% overall - and up to 82% in the first 30 days. A 72-year-old patient with borderline kidney function (eGFR 58 mL/min/1.73m²) developed severe kidney failure within 72 hours of starting ibuprofen while already taking lisinopril and furosemide. He didn’t feel sick until his legs swelled and he stopped urinating. By then, his eGFR had dropped to 22.
Who’s at Highest Risk?
Not everyone who takes NSAIDs will get kidney damage. But some groups are far more vulnerable:
- People over 65 - kidney function naturally declines with age.
- Those with chronic kidney disease (CKD), especially with eGFR below 60.
- People with heart failure, liver cirrhosis, or diabetes.
- Anyone dehydrated - from illness, heat, or exercise.
- Patients on diuretics, ACE inhibitors, or ARBs.
Even people who think they’re healthy can be at risk. A 2023 study found that 1 in 5 adults over 50 have undiagnosed early-stage kidney disease. They might feel fine, but their kidneys are already working harder than they should. Adding an NSAID can push them over the edge.
What About Acetaminophen or Opioids?
If NSAIDs are risky, what can you take instead?
Acetaminophen (Tylenol) is the most common alternative. It doesn’t affect kidney blood flow the same way NSAIDs do. Studies show it carries 40-50% less risk of acute kidney injury. But it’s not perfect - it can harm the liver if taken in excess, especially with alcohol or in people with liver disease. Stick to the lowest effective dose: no more than 3,000 mg per day.
Opioids don’t harm the kidneys directly, but they come with major downsides: addiction risk (15-25% with long-term use), constipation, drowsiness, and tolerance. They’re not a solution for everyday pain like arthritis or back pain. They’re meant for short-term, severe pain - like after surgery or a broken bone.
For localized pain - say, a sore knee or shoulder - topical NSAIDs (gels, creams, patches) are a smart choice. They deliver the pain relief right where it’s needed, with 70-80% less drug entering your bloodstream. A 2024 JAMA trial found they reduced kidney injury risk by 40-50% compared to pills.
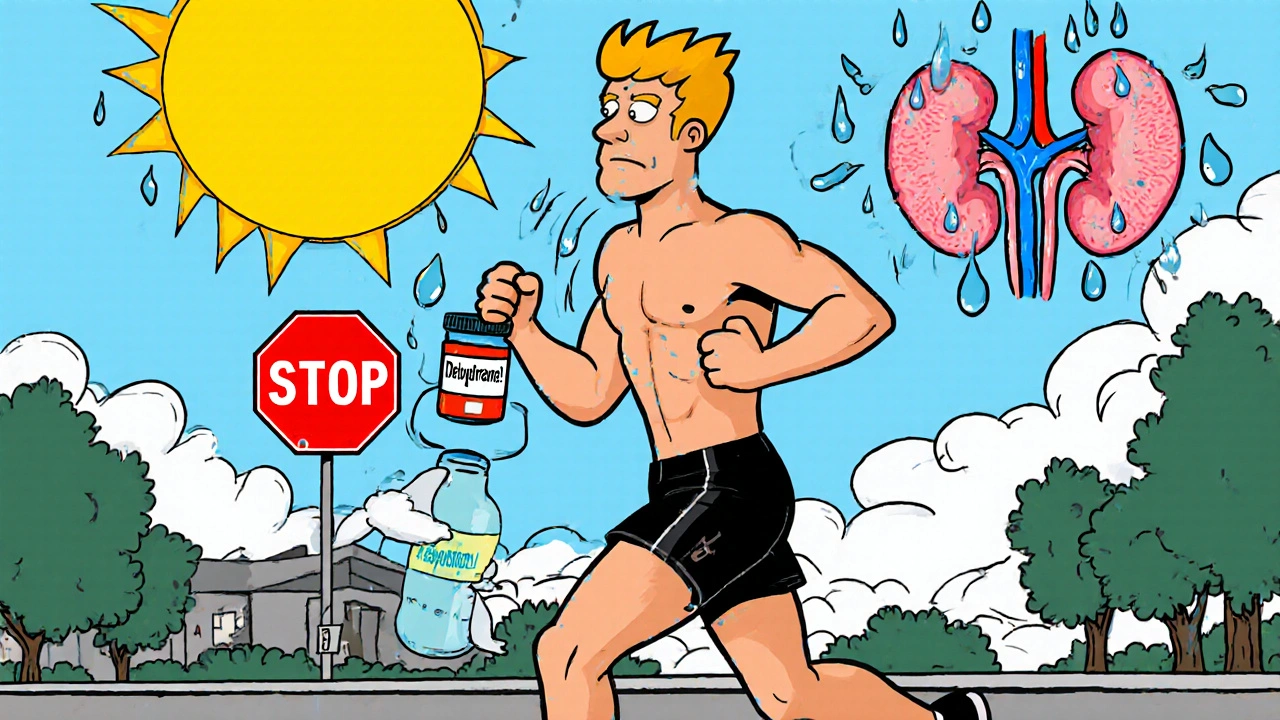
Exercise, Heat, and NSAIDs: A Dangerous Mix
Many runners and athletes take NSAIDs before or after long workouts, thinking it prevents soreness. But during exercise, your body redirects blood flow away from your kidneys to your muscles. Add dehydration, heat, and an NSAID, and you’re cutting off kidney blood flow from two sides.
A 2006 study found NSAID use during marathons can reduce renal blood flow by 30-50% beyond the normal drop from exercise alone. While only about 1 in 100,000 runners develops acute kidney injury this way, the cases that do happen are often severe. Hydration is key: drink 5-10 mL of fluid per kg of body weight 2-4 hours before exercise, and 0.4-0.8 liters per hour during activity. Keep your urine clear or pale yellow - if it’s dark, you’re dehydrated and shouldn’t be taking NSAIDs.
How to Stay Safe: A Practical Guide
If you have kidney disease or are at risk, here’s what you need to do:
- Know your eGFR. Ask your doctor for your estimated glomerular filtration rate. If it’s below 60, NSAIDs should be used with extreme caution. If it’s below 30, avoid them entirely.
- Avoid the triple whammy. Never take NSAIDs with ACE inhibitors, ARBs, and diuretics at the same time. If you’re on any of these, talk to your doctor before taking any OTC painkiller.
- Use the lowest dose for the shortest time. Don’t take NSAIDs daily unless absolutely necessary. For acute pain, limit use to 3-5 days. If pain lasts longer, see a doctor - don’t just keep taking more pills.
- Stay hydrated. Drink water consistently, especially if you’re sick, sweating, or in hot weather.
- Watch for warning signs. Decreased urine output, swelling in ankles or feet, unexplained fatigue, nausea, or confusion can all signal kidney trouble. Don’t wait for a blood test - if you feel off, get checked.
What’s Changing in 2025?
The medical community is finally catching up. In 2023, the American Society of Nephrology launched the NSAID-RF Risk Calculator - a tool that uses 12 factors like age, blood pressure, and current medications to predict your personal risk of kidney injury within 30 days. It’s not yet in every doctor’s office, but it’s a step toward personalized care.
Researchers are also testing new formulations - like ibuprofen combined with acetylcysteine - that may protect the kidneys while still relieving pain. Early trials show promise. And in 2025, a breakthrough in genetics identified specific gene variants (in the PTGS2 gene) that make some people far more sensitive to NSAID kidney damage. Soon, a simple blood test could tell you if you’re genetically at higher risk.
Right now, the best protection is awareness. NSAIDs aren’t evil. They’re powerful tools. But like any tool, they’re dangerous in the wrong hands - or the wrong body.
Frequently Asked Questions
Can I take ibuprofen if I have mild kidney disease?
If your eGFR is between 30 and 60 mL/min/1.73m², NSAIDs like ibuprofen should be used only if absolutely necessary, at the lowest possible dose, and for no more than 3 days at a time. Always check with your doctor first. Many people with mild kidney disease can safely use acetaminophen instead. If you must use an NSAID, avoid combining it with diuretics or blood pressure meds like ACE inhibitors or ARBs.
Do all NSAIDs affect the kidneys the same way?
No. Non-selective NSAIDs like ibuprofen and naproxen carry higher kidney risks than selective COX-2 inhibitors like celecoxib. But even celecoxib isn’t safe for people with eGFR below 60. The difference in risk is small - about 20-30% lower for COX-2 inhibitors - and it disappears in people with existing kidney disease. The safest option is often not taking any NSAID at all.
I’ve been taking naproxen for years for arthritis. Should I stop?
If you’ve been taking naproxen daily for years, especially if you’re over 60 or have high blood pressure or diabetes, you should talk to your doctor about switching. Long-term NSAID use increases your risk of chronic kidney disease progression by 50%. Many people develop kidney damage slowly over time without symptoms. A simple eGFR test and urine albumin test can show if your kidneys have been affected. Your doctor can help you find safer long-term pain options, like physical therapy, topical treatments, or low-dose acetaminophen.
Can NSAIDs cause permanent kidney damage?
Yes. While many cases of NSAID-induced acute kidney injury are reversible if caught early, repeated episodes or prolonged use can lead to permanent loss of kidney function. In people with pre-existing kidney disease, each NSAID-related injury can accelerate progression to end-stage kidney disease. Studies show chronic NSAID users are 67% more likely to see their kidney disease worsen compared to non-users.
Why don’t doctors warn patients more often?
Many doctors assume patients know NSAIDs are risky, or they don’t realize how common kidney disease is in older adults. Patient surveys show 72% of people who developed NSAID-related kidney injury say their doctor never warned them. Over-the-counter labels are vague, and many people assume “OTC” means “completely safe.” It’s a gap in communication - not a lack of evidence. If you’re over 50 or have any chronic condition, always ask your doctor or pharmacist about kidney risks before taking any new medication, even if it’s sold without a prescription.
Next Steps
If you’re taking NSAIDs regularly and have any risk factors - age, high blood pressure, diabetes, or a history of kidney issues - schedule a simple blood test to check your eGFR. Ask your doctor about urine albumin-to-creatinine ratio too. Both are cheap, non-invasive, and can catch early kidney damage before symptoms appear.
If you’re managing chronic pain, ask about alternatives: topical NSAIDs, physical therapy, low-dose acetaminophen, or even nerve blocks. Don’t wait until your kidneys are in crisis. Prevention isn’t about avoiding all pain relief - it’s about choosing the safest path.

Simone Wood
November 20, 2025 AT 19:28NSAIDs are basically silent killers for kidneys and no one talks about it. I had a cousin on lisinopril and ibuprofen for years-thought she was fine until she collapsed. eGFR dropped to 19 in 72 hours. No warning. No symptoms. Just… gone. Doctors don’t care until it’s too late. OTC doesn’t mean safe. It means you’re on your own.
Swati Jain
November 22, 2025 AT 14:41Let me break this down like I’m explaining it to my 70-year-old mom who thinks Tylenol is ‘just sugar pills’-NSAIDs don’t just hurt kidneys, they sabotage the backup system. Prostaglandins? Think of them as your kidney’s emergency oxygen mask. NSAIDs yank it out. ACE inhibitors? They’re the ones lowering the pressure. Diuretics? They’re draining the tank. Together? You’re flying a plane with both engines off and no fuel. And yes, I’ve seen this in clinics in Mumbai. It’s not a US problem. It’s a global silent epidemic.
Florian Moser
November 22, 2025 AT 20:53This is one of the most important public health messages in years. I’m a physical therapist and I see patients daily who take ibuprofen every day for ‘just a little ache.’ They don’t realize they’re slowly grinding down their kidneys. The key takeaway? If you’re over 50, have hypertension, diabetes, or are on any blood pressure meds-stop self-medicating with NSAIDs. Talk to your doctor. Get an eGFR test. It’s a $15 blood test that could save your life. Prevention isn’t complicated-it’s just ignored.
jim cerqua
November 24, 2025 AT 19:22THIS IS A MASSIVE COVER-UP. The pharmaceutical industry knows this. They know NSAIDs are kidney bombs. They know the triple whammy kills. But they don’t put warning labels on the bottles because they’d lose billions. The FDA? They’re asleep. Doctors? Too busy to explain. And now they’re pushing ‘new formulations’ like acetylcysteine combos like it’s magic? No. It’s PR. They’re not fixing the problem-they’re packaging it better. And don’t get me started on how they market topical NSAIDs as ‘safe’-it’s still systemic absorption, just slower. This isn’t science. It’s corporate theater.
Donald Frantz
November 25, 2025 AT 09:35Interesting that the article mentions PTGS2 gene variants but doesn’t explain them. The PTGS2 gene encodes COX-2, right? So if you have certain SNPs-like rs5275 or rs689466-you’re more likely to have exaggerated prostaglandin suppression from NSAIDs. That means even ‘low-dose’ ibuprofen could trigger AKI in genetically susceptible people. We’re talking about pharmacogenomics here. Why isn’t this in the standard screening? Why aren’t pharmacies offering genotyping for chronic pain patients? This isn’t just about awareness-it’s about precision medicine being ignored.
Sammy Williams
November 25, 2025 AT 18:51My grandma’s on all three meds-lisinopril, furosemide, and takes naproxen every Sunday for her knees. I just told her to switch to the topical gel. She thought I was being dramatic. I showed her the JAMA study. Now she uses the patch and drinks more water. No more ‘just one pill’ after church. It’s scary how easy it is to accidentally poison yourself with stuff you buy at the gas station. Thanks for the wake-up call.
Julia Strothers
November 27, 2025 AT 08:53They’re lying to us. The CDC, the AMA, the FDA-they all know NSAIDs are killing elderly Americans by the thousands. Why? Because it’s cheaper to let people die than to force drug companies to change labels. And now they want us to trust ‘personalized risk calculators’? That’s just a fancy way of saying ‘we’re not going to ban it, so figure it out yourself.’ Meanwhile, the pharmaceutical lobby spends $100 million a year lobbying against warning labels. This isn’t negligence. It’s murder by bureaucracy.
Erika Sta. Maria
November 27, 2025 AT 11:16Wait… so acetaminophen is ‘safer’? But what about the liver? And what if you’re diabetic? And what if you drink? And what if you’re Asian? And what if you’re a woman? And what if you’re over 40? And what if you’ve had COVID? And what if you’re on SSRIs? And what if you’re… oh wait, EVERYTHING is dangerous. So what’s the point? Maybe we should just stop taking medicine altogether and meditate. Or maybe pain is just a spiritual lesson. Or maybe… we’re all just meat sacks waiting to fail. 🤷♀️