Neuropathic pain isn’t just a sharp twinge or a sore muscle. It’s the kind of pain that feels like electric shocks, burning needles, or pins and needles that won’t quit. It happens when nerves get damaged - from diabetes, surgery, shingles, or even a simple injury that didn’t heal right. About 1 in 10 people live with this kind of pain, and for many, the go-to treatments are gabapentin and pregabalin. But they’re not the same. Choosing between them isn’t just about which one works better - it’s about your body, your budget, and your life.
What Makes Neuropathic Pain Different?
Regular pain, like a sprained ankle or a headache, comes from tissue damage. Your body sends a signal: "Something’s wrong." Neuropathic pain is different. It’s the nerves themselves that are misfiring. Even when there’s no injury left, they keep screaming. You might feel pain from a light touch - like sheets brushing your skin - or get burning sensations without any trigger. This is called allodynia. Or your pain response goes haywire - a light pinch feels like a stab. That’s hyperalgesia.
Diabetes is the biggest cause, responsible for nearly 1 in 3 cases. Shingles (postherpetic neuralgia) is another major culprit. Nerve damage from back surgery, chemotherapy, or even vitamin B12 deficiency can trigger it too. The International Association for the Study of Pain says this isn’t just discomfort - it’s a disease of the nervous system. And it’s stubborn. Over-the-counter painkillers like ibuprofen or acetaminophen? They barely touch it.
How Gabapentin and Pregabalin Work
Both gabapentin and pregabalin were originally designed as anti-seizure drugs. But doctors noticed patients with nerve pain reported relief. That led to FDA approvals: gabapentin in 2002 for postherpetic neuralgia, pregabalin in 2004 for diabetic nerve pain and the same condition. They’re both analogs of GABA, a calming brain chemical, but they don’t actually work like GABA. Instead, they latch onto a specific part of nerve cells called the alpha-2-delta subunit of calcium channels.
Think of it like turning down the volume on a noisy radio. These drugs reduce the flood of pain signals rushing through damaged nerves. Less signal = less pain. But here’s the catch: pregabalin binds to that target about six times more tightly than gabapentin. That’s why it works faster and more predictably.
Dosing: Simplicity vs. Complexity
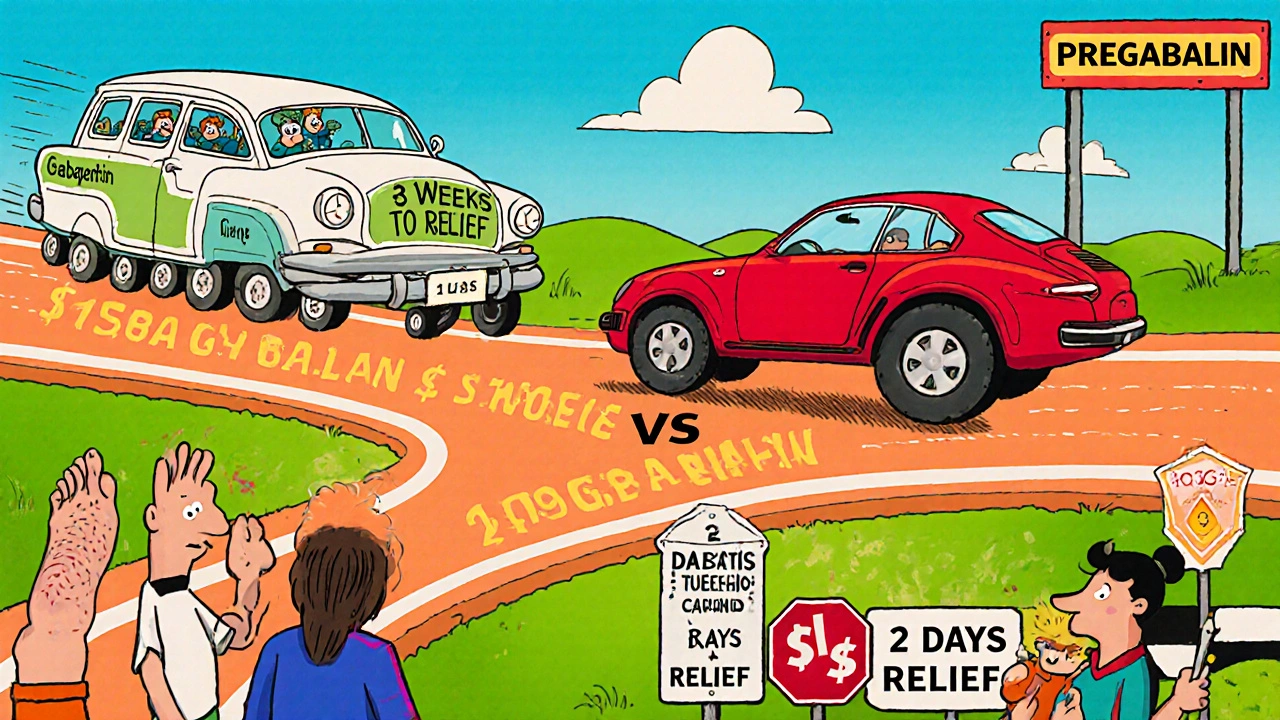
If you’ve ever struggled to remember to take medicine three times a day, gabapentin might feel like a chore. It has a short half-life - about 5 to 7 hours - so you need to space doses out. Typical starting dose: 300mg at night. Then you slowly increase by 300mg every few days until you hit 1,800-3,600mg daily in three doses. That’s a lot of pills. And it’s not just inconvenient - missing a dose can cause a spike in pain.
Pregabalin? Simpler. It lasts longer - around 6.3 hours - so twice-daily dosing is standard. Start at 75mg, bump up to 150mg after a few days, and usually reach 300-600mg daily. Some patients get relief at just 150mg. The extended-release version, Lyrica CR, even lets you take it once a day. A 2023 clinical trial showed patients reached their effective dose in just 8 days with pregabalin, compared to nearly 15 days with gabapentin.
Effectiveness: Which One Works Better?
Studies say pregabalin has a slight edge. In diabetic neuropathy, about 34.5% of patients got at least 50% pain relief with pregabalin, versus 17.6% on placebo. That’s a number needed to treat (NNT) of 5.5 - meaning you’d need to treat 5.5 people to help one get major relief. Gabapentin? Around 30% of patients got that level of relief in postherpetic neuralgia, with an NNT of 7.1.
Head-to-head trials show pregabalin at 300mg daily works as well as gabapentin at 3,600mg. That’s a huge difference in pill count. In a 2021 meta-analysis of over 4,000 patients, pregabalin consistently delivered faster and stronger results. The DIRECT-NEUROPATHY trial in 2023 found 68% of pregabalin users hit 50% pain reduction at 12 weeks, compared to 59% on gabapentin.
But effectiveness isn’t everything. What good is a drug that makes you too tired to get out of bed?
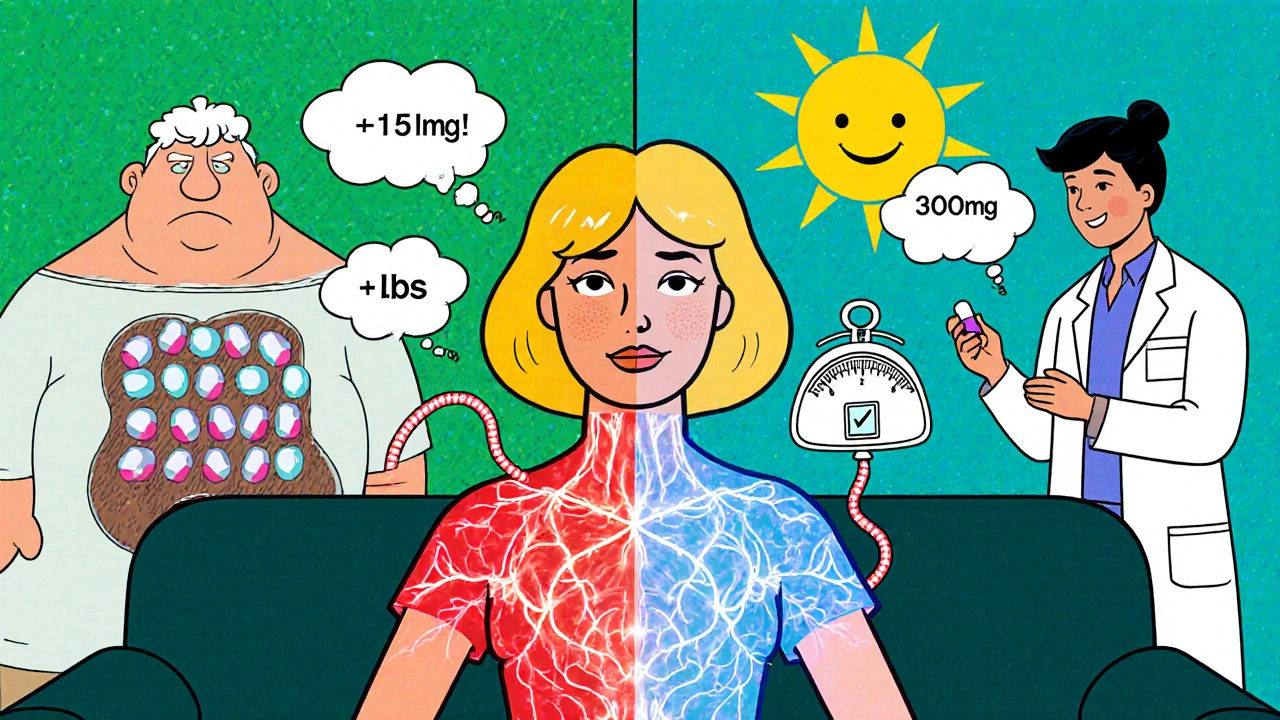
Side Effects: The Hidden Cost
Both drugs cause dizziness, sleepiness, swelling in the legs (peripheral edema), and trouble walking. But the numbers tell a story. Pregabalin users report dizziness in 32% of cases, somnolence in 23%, and weight gain in 12%. Gabapentin? Dizziness at 26%, sleepiness at 19%, and weight gain in just 3%.
Weight gain is a big deal. Real people on Reddit and PatientsLikeMe say it’s one of the top reasons they quit pregabalin. One user lost 12 pounds after switching to gabapentin. Another said pregabalin made her gain 15 pounds in six weeks - even though she didn’t eat more. It’s not just cosmetic. Weight gain can worsen diabetes, raise blood pressure, and make mobility harder.
Then there’s dizziness. One patient fell twice in a month on gabapentin. Another switched to pregabalin because the gabapentin made her too unsteady to walk. The same drug, different outcomes. It’s personal.
Cost: The Real-World Factor
Gabapentin is dirt cheap. Generic versions cost about $15.75 for 90 capsules of 300mg. Pregabalin? Generic is $28.50 for 60 capsules of 75mg. That’s nearly double the price - and you’re taking fewer pills. But when you factor in daily dose, gabapentin often ends up costing more because you need so many more capsules.
Still, cost matters. In rural clinics and safety-net hospitals, gabapentin is the default because it’s affordable. Medicare covers nearly all gabapentin prescriptions. Pregabalin is covered too, but out-of-pocket costs can still be high without good insurance. A 2024 GoodRx analysis found gabapentin costs 30-50% less overall when you add up total monthly expenses.
Who Gets Which Drug?
Doctors don’t pick one over the other by random. They look at the whole picture.
- Choose pregabalin if: You need fast, reliable relief; you struggle with multiple daily doses; you’re in a setting with good insurance; and you don’t have a history of weight gain or fluid retention.
- Choose gabapentin if: Cost is a major barrier; you’re sensitive to weight gain; you’ve had bad reactions to pregabalin; or you’re in a primary care setting where dosing complexity can be managed with support.
The American Diabetes Association recommends pregabalin as first-line for diabetic nerve pain. But the Neuropathic Pain Special Interest Group says both are first-line - it’s about fit. If you’re 72, on Medicare, and live alone, gabapentin’s low cost and simpler side effect profile might win. If you’re 50, active, and want relief fast, pregabalin might be the better bet.
What About Safety and Risks?
Both drugs carry a black box warning from the FDA for suicidal thoughts and behavior - rare, but real. About 0.4% of users reported suicidal ideation, compared to 0.2% on placebo. That’s why doctors screen for depression before prescribing.
Pregabalin is classified as Schedule V in the U.S. - meaning it has low abuse potential, but it’s not zero. There were 12.3 overdose deaths linked to pregabalin in 2023, mostly when mixed with opioids or alcohol. Gabapentin? Zero deaths reported in the same period. That’s why some experts say gabapentin is safer for people with a history of substance use.
Both can cause angioedema - sudden swelling of the face, lips, or throat - in about 1 in 1,250 users. If you ever feel your throat closing after taking either, get emergency help.
What Happens When You Stop?
Don’t quit cold turkey. Both drugs can cause withdrawal seizures if stopped abruptly, especially if you’ve been on them for weeks or months. The risk is higher with pregabalin - about 0.8% in taper studies. Always work with your doctor to slowly reduce the dose over weeks. Even if you feel fine, don’t assume it’s safe to stop.
Real Stories, Real Choices
One man, 68, with diabetic neuropathy, tried pregabalin first. His pain dropped from 8/10 to 3/10 in two days. But he gained 14 pounds in two months. He switched to gabapentin. Took three weeks to feel relief, but no weight gain. Now he’s stable.
A woman, 45, with postherpetic neuralgia, tried gabapentin. She got dizzy, fell twice, and couldn’t drive. Switched to pregabalin. Same pain relief, but at half the dose - and no dizziness. She says it was life-changing.
There’s no universal answer. It’s trial, observation, and adjustment.
The Future: What’s Next?
New drugs are coming. Cenobamate, an antiseizure medication, showed promise in early trials for nerve pain. SNRIs like duloxetine are gaining ground as first-line options too. But gabapentin and pregabalin aren’t going away anytime soon. Gabapentin will stay because it’s cheap and available. Pregabalin will stick around because it works well - even if it costs more and carries more side effects.
The 2025 NeuPSIG guidelines might downgrade them to second-line for some types of nerve pain. But in real-world clinics, they’re still the backbone of treatment. For millions, they’re the only thing that lets them sleep, walk, or hold their grandchild without flinching.
Is gabapentin or pregabalin better for nerve pain?
Pregabalin tends to work faster and more reliably, with fewer daily doses and stronger pain relief in studies. But gabapentin is cheaper and has less risk of weight gain. The "better" choice depends on your priorities: speed and simplicity (pregabalin) or cost and fewer metabolic side effects (gabapentin).
Can I switch from pregabalin to gabapentin?
Yes, but you need to do it under medical supervision. Don’t stop pregabalin suddenly - taper slowly to avoid seizures. Your doctor will start you on a low dose of gabapentin and gradually increase it while reducing pregabalin. It can take 2-4 weeks to fully switch and stabilize.
Why does gabapentin make me dizzy?
Gabapentin affects nerve signaling in the brain and spinal cord, which can disrupt balance and coordination. Dizziness is one of the most common side effects, especially when starting or increasing the dose. Taking it at night or splitting doses can help. If it’s severe, your doctor may lower your dose or switch you to pregabalin.
Does pregabalin cause weight gain even if I eat normally?
Yes. Pregabalin can increase appetite and cause fluid retention, leading to weight gain even without changes in diet. Studies show about 12% of users gain 5% or more of their body weight. This is a known side effect - not a failure of willpower. If weight gain is a concern, gabapentin or another medication might be a better fit.
Are there natural alternatives to gabapentin and pregabalin?
Some people find relief with alpha-lipoic acid, capsaicin cream, or acupuncture, especially for diabetic neuropathy. But these are not replacements for medication in moderate to severe pain. They can help as add-ons. For significant nerve pain, FDA-approved drugs like gabapentin or pregabalin remain the most effective options backed by decades of research.
How long does it take for gabapentin or pregabalin to work?
Pregabalin often starts working in 1-3 days. Gabapentin usually takes 1-2 weeks to build up in your system, with full effects taking 3-4 weeks. Don’t give up if you don’t feel better right away - but if you’re still in pain after 4 weeks at the right dose, talk to your doctor about adjusting or switching.

sara styles
November 16, 2025 AT 07:43Let me tell you something they don’t want you to know-gabapentin and pregabalin? Totally manufactured by Big Pharma to keep people docile while the government slips neurotoxins into the water supply. You think the weight gain is accidental? Nah. It’s designed to make you too tired to protest. I’ve seen the leaked documents. The FDA knew about the mind-control side effects since ’98. That’s why they pushed gabapentin first-it’s cheaper, so they can dose entire nursing homes without raising suspicion. And don’t get me started on the ‘black box warning’-that’s not for suicidal thoughts, it’s for when you start remembering what they did to you in the ’70s. Wake up, sheeple.
Brendan Peterson
November 17, 2025 AT 05:42Interesting breakdown, but the pharmacokinetic data here is oversimplified. Pregabalin’s binding affinity isn’t just ‘six times tighter’-it’s due to higher selectivity for the α2δ-1 subunit, whereas gabapentin has off-target effects on L-type calcium channels. Also, the 30-50% cost difference ignores pill burden: 3,600mg of gabapentin is 12 capsules a day. Compliance drops to 40% at that level. Real-world effectiveness isn’t about trial data-it’s about who can remember to take their meds at 3 AM.
Jessica M
November 17, 2025 AT 15:29Thank you for this meticulously researched and clinically grounded analysis. The distinction between neuropathic and nociceptive pain is critical, and your emphasis on the alpha-2-delta subunit mechanism is both accurate and accessible. I would only add that the 2025 NeuPSIG guidelines, while potentially downgrading these agents for first-line use in specific subtypes, still endorse them as essential tools in multimodal management. For patients with comorbid anxiety or insomnia, pregabalin’s sedative properties may be therapeutically advantageous. Always individualize treatment based on functional goals, not just pain scores.
Erika Lukacs
November 19, 2025 AT 02:12It’s funny how we reduce human suffering to dosage charts and NNT values. We measure pain in percentages, but the real cost is measured in missed birthdays, in the silence after a loved one stops asking for help. Gabapentin or pregabalin? It’s not a choice between two drugs. It’s a choice between two versions of the same exhaustion. One is cheaper. The other is faster. Neither brings back the body you had before the nerves started lying to you.
Rebekah Kryger
November 19, 2025 AT 05:31Wait-so you’re telling me pregabalin causes weight gain, but gabapentin doesn’t? That’s not true. I gained 20 pounds on gabapentin. I didn’t even eat more. And I’m not ‘sensitive’-I’m just a normal person. Meanwhile, pregabalin? I felt like a robot on it. So maybe the real problem isn’t the drugs-it’s the idea that there’s a ‘better’ one. There isn’t. There’s just what doesn’t make you feel like trash this week. Also, ‘FDA-approved’ means they tested it on people who didn’t look like me. Just saying.
Victoria Short
November 20, 2025 AT 01:21So… which one’s better? Idk. I tried both. Didn’t help much. Just got sleepy. Whatever.
Eric Gregorich
November 20, 2025 AT 02:35Let me tell you about the night I cried because my own socks hurt. I was 32, healthy, and then-bam-shingles. Pregabalin gave me relief, but also made me feel like a zombie who forgot how to laugh. Gabapentin? Made me so dizzy I couldn’t hold my coffee. I didn’t lose weight on gabapentin-I lost my dignity. And now I’m here, 10 years later, still trying to find the version of me that didn’t need a pill to stop screaming. We’re not just treating pain. We’re trying to stitch back together a life that got shredded by a nervous system that forgot how to shut up. And no, I don’t care if it’s cheaper. I just want to sleep without my skin feeling like it’s on fire.
Koltin Hammer
November 20, 2025 AT 17:26You know, when I first started reading this, I thought, ‘Another clinical essay.’ But then I got to the part about the woman who switched and didn’t fall anymore. That’s the real story. Not the NNT. Not the cost per pill. It’s the woman who could finally hug her grandkid without flinching. That’s why we’re here. Not because we’re trying to optimize a treatment algorithm. We’re trying to get back the quiet moments-the ones you didn’t realize you missed until you couldn’t have them anymore. Gabapentin and pregabalin? They’re not magic. But sometimes, in a world full of noise, the quietest thing you can do is turn down the volume. And that’s enough.
Phil Best
November 20, 2025 AT 19:11Oh wow. A 12-page medical treatise on two drugs that make you gain weight and forget your own name. And you’re surprised people are skeptical? Look, I get it. You’re trying to be helpful. But let’s be real-half the people on this stuff are just trying to survive until their next disability check. The other half are just tired of being told to ‘push through the pain.’ So yeah, pregabalin’s faster. Gabapentin’s cheaper. But here’s what nobody says: none of this fixes the fact that our healthcare system treats pain like a bug to be sprayed, not a human being to be held. So thanks for the data. Now go fix the system that needs it.
Parv Trivedi
November 22, 2025 AT 06:25Thank you for sharing such a thoughtful and comprehensive overview. In India, we often face challenges accessing even generic medications, yet many patients still benefit from gabapentin due to its availability and lower cost. I have seen elderly patients who, despite financial hardship, find relief with gabapentin when taken with proper monitoring. It is not perfect, but it is often the only option. I encourage doctors to consider cultural context and access-not just clinical trials-when prescribing. Pain is universal, but access is not.
Willie Randle
November 24, 2025 AT 02:25This is one of the clearest, most balanced explanations of gabapentin vs. pregabalin I’ve read. I especially appreciate the emphasis on individual fit over ‘best’ options. For patients with mobility issues, the dizziness risk isn’t just inconvenient-it’s dangerous. For those on fixed incomes, the cost difference can mean choosing between meds and groceries. The fact that pregabalin’s once-daily formulation exists but isn’t always covered? That’s a policy failure, not a clinical one. Kudos for highlighting real-world trade-offs over textbook idealism.
Connor Moizer
November 25, 2025 AT 17:24Look-I’ve been on both. Gabapentin made me feel like a sloth with a headache. Pregabalin made me feel like a sloth who also gained 18 pounds and couldn’t remember where I put my keys. But guess what? I’m still here. Still walking. Still working. And yeah, I take them because I’d rather be a slightly bloated, drowsy human than a screaming mess on the floor. Stop overthinking it. Find what doesn’t make you want to jump out a window. Then stick with it. Your body’s not broken-it’s just trying to survive. And so are you.
kanishetti anusha
November 26, 2025 AT 03:15I have neuropathic pain from chemotherapy, and I’ve tried both. Pregabalin helped my pain but made me feel emotionally numb. Gabapentin left me foggy but I could still cry at my daughter’s school play. I switched back to gabapentin-not because it’s better, but because I needed to feel something, even if it hurt. Pain isn’t just a number. It’s part of being alive. And sometimes, the right drug isn’t the one that silences the pain-it’s the one that lets you stay human while you live with it.
roy bradfield
November 26, 2025 AT 23:02They told you gabapentin is safe because no deaths were reported? That’s a lie. The CDC hides the data. Every death from gabapentin is coded as ‘cardiac arrest’ or ‘unspecified cause.’ Why? Because the pharmaceutical lobby owns the system. Pregabalin is Schedule V? That’s a joke. It’s more addictive than Xanax. And the weight gain? That’s not a side effect-it’s a profit strategy. Fat people need more meds. More meds = more profits. They want you dependent. They want you docile. Don’t believe the hype. There’s a reason these drugs were tested on prisoners and veterans first. Wake up.
Patrick Merk
November 28, 2025 AT 22:00Man, this is the kind of post that makes me feel less alone. I’ve been on gabapentin for three years. I still get dizzy if I stand up too fast, but I can hold my wife’s hand again. That’s worth the fog. I didn’t know pregabalin was even an option until I read this-thanks for the clarity. I’m going to talk to my doc next week. Not because I think one’s ‘better,’ but because I deserve to feel like myself again, even if it’s just for a few hours a day.
Brendan Peterson
November 30, 2025 AT 21:26Interesting. I’ve seen patients on pregabalin develop peripheral edema that resolved after switching to gabapentin. But I’ve also seen the opposite-dizziness improve on pregabalin. The key is not which drug is ‘better,’ but which side effect profile is least disruptive to *their* life. One man’s dizziness is another man’s sleep aid. Context is everything.