When you pick up a bottle of liquid amoxicillin for your child, it looks fresh. The label says "use within 14 days." But why? Why can’t you keep it longer? Why does your pharmacist hand you a tiny bottle with a discard date scrawled on it like it’s a perishable milk carton? The answer isn’t about quality control or corporate greed-it’s chemistry. And it’s urgent.
Why Liquid Antibiotics Don’t Last
Powdered antibiotics are stable. They sit on shelves for years. But as soon as you add water, everything changes. The moment you reconstitute amoxicillin, ampicillin, or any beta-lactam antibiotic, water starts breaking down the chemical structure. This isn’t slow decay-it’s a targeted chemical reaction called hydrolysis. The beta-lactam ring, the part of the molecule that kills bacteria, unravels in water. Once that happens, the drug loses its power. You’re not just wasting medicine-you’re risking treatment failure.Studies show that after 14 days in the fridge, amoxicillin drops below 90% of its labeled potency. That’s not a random number. It’s the FDA’s minimum standard for safety and effectiveness. Below that, you’re not treating the infection-you’re just feeding bacteria that learn to survive.
Amoxicillin vs. Amoxicillin-Clavulanate: The Stability Difference
Not all liquid antibiotics are the same. Amoxicillin alone? It can last up to 14 days in the refrigerator. But add clavulanate-the part that blocks resistant bacteria-and suddenly, you’re down to 10 days. Why? Clavulanate is even more fragile. It breaks down faster than amoxicillin, especially when exposed to heat or stored in plastic oral syringes.One study found that when clavulanate was transferred from its original bottle into a plastic syringe, its stability dropped from 11 days to under 5 days-even when kept cold. That’s not a myth. That’s lab data. Many parents don’t know this. They pour the liquid into a syringe for easier dosing and assume it’s fine. It’s not.
Temperature Is Everything
Refrigeration isn’t optional. It’s mandatory. Store your liquid antibiotic at room temperature, and you cut its life in half. At 27°C (80°F), amoxicillin-clavulanate loses potency in just five days. At 5°C (41°F)? Ten to fourteen days. Every 10°C increase doubles the degradation rate. That’s not a guess-it’s Arrhenius kinetics, a well-established chemical rule.Many families forget to refrigerate. Maybe the bottle sat on the counter while the child slept. Maybe it was left in a warm car. That tiny lapse could mean the difference between healing and a stubborn, recurring infection. Pharmacists report that 40% of returned bottles are from parents who didn’t refrigerate properly.

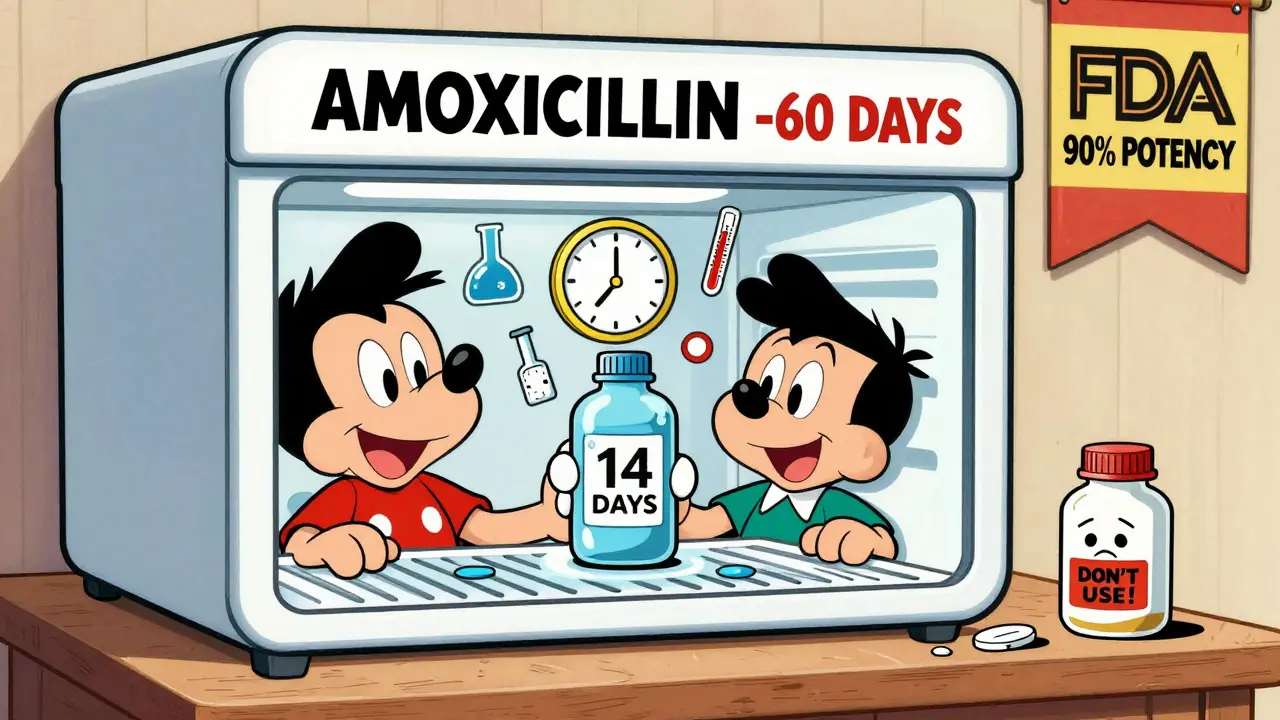
Freezing: A Hidden Option
Most people don’t know you can freeze liquid antibiotics. Yes, really. Studies from the 1970s show that amoxicillin and penicillin V potassium retain over 90% potency for up to 60 days when stored at -20°C. That’s two months. But here’s the catch: not all pharmacies offer this. And once thawed, you can’t refreeze it. The stability clock resets.If your child needs a 14-day course and the prescription runs out before the antibiotic does, ask your pharmacist about freezing. Some will do it if you ask. Others won’t. But the science is clear: freezing works. It’s not a hack-it’s a proven method endorsed by hospital pharmacies for decades.
What Happens If You Use Expired Liquid Antibiotics?
You won’t get sick from a bad antibiotic. You won’t suddenly develop poisoning. But you might not get better. The bacteria keep growing. The infection lingers. You come back to the doctor, who prescribes another round. And another. Each time, the bacteria get stronger. That’s how antibiotic resistance starts-not from overuse alone, but from underdosing.One parent on a health forum shared that her child’s ear infection came back after 10 days because they’d thrown out the medicine too early. Another admitted they kept using the bottle past the 14-day mark because “it still looked fine.” It did. But it wasn’t working. The color didn’t change. It didn’t smell bad. But the active ingredient? Gone.
How to Avoid the Mistakes
Here’s what actually works:- Write the discard date on the bottle the second you get it. Don’t wait. Don’t trust your memory. Use a permanent marker.
- Keep it refrigerated at 2-8°C. Not the fridge door. The back shelf. That’s where it’s coldest.
- Don’t transfer to syringes unless you must. If you do, use glass or high-quality plastic, and discard after 5 days.
- Check for changes. Cloudiness, lumps, odd smell? Toss it. Even if it’s day 3.
- Ask about freezing. Especially if the course is longer than 10 days.
Some pharmacies now use reminder apps that text you when the discard date hits. CVS’s Script Sync reduced improper use by 18% in their 2022 audit. If your pharmacy doesn’t offer this, ask them to. It’s a simple fix.
The Bigger Picture
Liquid antibiotics make up about 15% of all antibiotic prescriptions in the U.S.-mostly for kids. But the industry knows the problem. New formulations are coming. Pfizer’s AmoxiClick system, launching in 2024, keeps the powder and liquid separate until you press a button. That could extend shelf life to 30 days. Other companies are testing microencapsulation that delays degradation.But until then? The rules are simple: refrigerate. Write the date. Don’t stretch it. Your child’s health depends on it-not on hope, not on convenience, but on chemistry that doesn’t lie.
What to Do If You’ve Already Used Expired Antibiotics
If you accidentally gave your child medicine past the discard date, don’t panic. But don’t ignore it either. Call your pharmacist or pediatrician. Tell them when you opened it, how you stored it, and how much you gave. They’ll help you decide whether to restart the course or switch treatments.Don’t feel guilty. This happens to a lot of families. The real mistake isn’t using it past the date-it’s not knowing the rules in the first place. Now you do.
How long does liquid amoxicillin last after reconstitution?
Refrigerated liquid amoxicillin lasts up to 14 days. Amoxicillin-clavulanate lasts only 10 days. At room temperature, both lose potency after 5-7 days. Always check the label-some brands vary slightly.
Can I freeze liquid antibiotics to make them last longer?
Yes. Studies show amoxicillin and penicillin V potassium retain potency for up to 60 days when frozen at -20°C. Not all pharmacies offer this service, but it’s safe and scientifically valid. Once thawed, use within 14 days and never refreeze.
Why does amoxicillin-clavulanate expire faster than plain amoxicillin?
Clavulanate is chemically unstable in water. It breaks down faster than amoxicillin, even when refrigerated. This is why combination drugs like Augmentin have a 10-day shelf life, while plain amoxicillin lasts 14 days. The clavulanate component is the weak link.
Is it safe to use liquid antibiotics after the discard date if they look fine?
No. Antibiotics don’t always look or smell bad when they expire. The active ingredient degrades invisibly. Even if the liquid is clear and smells normal, it may have lost enough potency to fail treatment. Never rely on appearance alone.
What should I do if my child’s antibiotic course is longer than the shelf life?
Talk to your pharmacist before starting. Ask if freezing is an option. Some pharmacies will reconstitute a second bottle to cover the full course. Others may prescribe a new batch with a fresh discard date. Never stretch one bottle beyond its limits.
Do I need to throw away unused liquid antibiotics after the discard date?
Yes. Even if it’s only half gone, discard it. Don’t save it for next time. Antibiotics are not like pain relievers-they’re targeted treatments. Using degraded antibiotics contributes to resistance and can make future infections harder to treat.
If you’re managing a child’s antibiotic treatment, treat the bottle like a fresh meal-store it right, use it on time, and don’t risk leftovers. Your child’s recovery depends on every drop working exactly as it should.



Trevor Whipple
January 14, 2026 AT 09:02so like… i just read this and i’m like wow i’ve been doing it wrong for years. i mean, i’ve totally left amoxicillin on the counter because my kid wouldn’t drink it unless it was room temp. like, who knew water was just slowly murderin’ the medicine? lol. also, why do pharmacies even give us these tiny bottles? like, 14 days? my kid’s infection lasted 3 weeks. why not just make it last longer??
Lethabo Phalafala
January 15, 2026 AT 10:43OH MY GOD. I JUST REALIZED I DID THIS. MY DAUGHTER HAD AN EAR INFECTION LAST YEAR AND I KEPT THE BOTTLE BECAUSE IT LOOKED FINE. I THOUGHT IT WAS JUST ‘WASTED’ IF I THREW IT OUT. NOW I FEEL LIKE A TERRIBLE MOM. I’M CALLING MY PHARMACY RIGHT NOW TO ASK ABOUT FREEZING. THIS IS LIFE-CHANGING INFO. THANK YOU FOR WRITING THIS. I’M CRYING. 😭
Lance Nickie
January 16, 2026 AT 04:09nah bro. it’s not chemistry. it’s just the pharma companies makin’ money. they want you to buy new bottles. period.
Milla Masliy
January 18, 2026 AT 02:01As someone raised in a household where medicine was never wasted - even if it was 2 months past the date - this hit different. My grandmother used to say, ‘If it looks right, it works right.’ But now I see… it’s not about looks. It’s about invisible science. I’m gonna start writing dates on every bottle. And I’m asking my pharmacist about freezing. Thank you for normalizing this conversation.
Damario Brown
January 20, 2026 AT 00:23you guys are all missing the real issue. the 14-day rule is a corporate lie. the FDA doesn't care about efficacy. they care about liability. if you give a kid 80% potency and he gets worse, the pharmacy gets sued. so they cap it at 14 days to cover their asses. the real degradation curve? it's linear, not exponential. you could probably use it for 21 days if refrigerated. but no one wants to be the first to test that. so we all just follow the script. also, clavulanate is a joke. it's like putting a tissue over a hurricane. it's not even designed to last. the whole system is broken.
sam abas
January 20, 2026 AT 14:37ok but let’s be real - this whole thing is just a glorified placebo effect wrapped in jargon. i’ve given my kid amoxicillin past the date 3 times. he got better. the bacteria didn’t evolve. the infection cleared. why? because the immune system does 80% of the work. the antibiotic is just a nudge. also, the ‘90% potency’ standard? that’s arbitrary. why not 85%? or 70%? the FDA doesn’t even test real-world conditions. they test in sterile labs with perfect refrigeration. in the real world, kids spill it, leave it out, shake it, drop it. so why pretend this is some precise science? it’s not. it’s fear-based compliance. and it’s making parents paranoid.
John Pope
January 21, 2026 AT 12:10we live in a world where medicine is treated like artisanal kombucha. ‘oh, it’s alive, it’s breathing, it’s evolving!’ but no - it’s a molecule. a fragile, beautiful, tragic molecule. and we, as a species, have turned healing into a ritual of anxiety. we mark dates like sacred runes. we whisper to bottles in the fridge. we fear the invisible decay. but here’s the truth: nature doesn’t care about your discard label. bacteria don’t read FDA guidelines. they just multiply. and maybe - just maybe - the real crisis isn’t expired antibiotics. it’s our desperate need to control everything, even the decay of chemicals we don’t understand.
Clay .Haeber
January 22, 2026 AT 00:15Wow. So the pharma giants are just… *dramatic gasp* … forcing us to buy more antibiotics by making them expire faster? And you’re telling me the solution is… writing on the bottle with a Sharpie? That’s the pinnacle of medical innovation? I mean, I’m impressed. Next they’ll tell us to pray to the fridge gods for optimal potency. 🙃 At least the new AmoxiClick system sounds like something from a sci-fi movie. Finally, someone’s thinking outside the plastic vial.
Priyanka Kumari
January 22, 2026 AT 23:56This is such an important post. In India, many parents reuse antibiotics because they’re expensive. We don’t have access to pharmacies that offer freezing or reminder apps. But now I know - even if we can’t freeze it, we must never stretch the course. I’m sharing this with my local moms’ group. Let’s stop the cycle of underdosing. One bottle, one course, one chance to heal right.
Avneet Singh
January 24, 2026 AT 17:56Let’s be honest - the entire concept of reconstituted antibiotics is a regulatory failure. The industry should be developing stable liquid formulations, not relying on 1970s freezing protocols. This is basic pharmaceutical science. Why are we still using glass bottles and manual labeling? The lack of innovation here is embarrassing. Also, ‘ask your pharmacist’? That’s not a solution. That’s a cop-out.
Adam Vella
January 25, 2026 AT 00:00While the chemical degradation of beta-lactam antibiotics is well-documented, the assertion that 90% potency is a clinical threshold is misleading. Clinical efficacy is not linearly correlated with potency. Sub-therapeutic dosing contributes to resistance, but the 90% figure is a regulatory artifact, not a biological one. Furthermore, the assumption that patients cannot discern clinical failure from antibiotic failure is patronizing. The real issue is access to timely medical follow-up - not refrigeration schedules.
Nelly Oruko
January 25, 2026 AT 08:14thank you for this. i’ve been scared to throw away medicine for years. i thought it was wasteful. now i get it: wasting it is the responsible thing. 🤍 i’ll write the date on the bottle. i’ll keep it in the back of the fridge. i won’t use the syringe. i promise.
vishnu priyanka
January 25, 2026 AT 22:44bro, i just gave my cousin’s kid amoxicillin that was 18 days old. it was still clear, still smelled like grape. he got better. but now i’m wondering… was i lucky? or was i just dumb? 🤔 maybe this post is the universe’s way of saying ‘stop winging it, man.’
Angel Tiestos lopez
January 27, 2026 AT 02:23ok but freezing antibiotics?? 🤯 that’s like putting your pizza in the freezer to make it last longer. it’s not wrong… but it feels like cheating. i’m gonna try it. also, why do we even need to reconstitute? why can’t they just make it ready to drink? like… is it cheaper to make powder? 🤔 i need answers. 🧪❄️
Alan Lin
January 28, 2026 AT 21:29As a pediatric nurse for 17 years, I’ve seen the consequences of expired antibiotics more times than I can count. Children with recurrent infections. Parents who feel guilty. Doctors who have to restart the entire course. This isn’t theoretical - it’s clinical reality. Refrigerate. Label. Don’t transfer to syringes unless necessary. And if you’re unsure - call your provider. Your child’s immune system can’t compensate for subtherapeutic dosing. This isn’t advice. It’s a protocol. Follow it.