Emergency Contraception Decision Guide
Select Your Situation
Answer a few questions to get personalized recommendations for emergency contraception options.
When you need emergency contraception (EC) fast, the choices on the shelf can feel overwhelming. The I-Pill is the most recognized brand of levonorgestrel, a synthetic hormone used to prevent pregnancy after unprotected sex or contraceptive failure. But it isn’t the only option. This guide breaks down how the I‑Pill stacks up against the main alternatives - ulipristal acetate, the copper IUD, the Yuzpe method and a few off‑label drugs - so you can pick the right backup plan for your body and lifestyle.
Why the I‑Pill is Often the First Choice
The I‑Pill works by delivering a high dose of levonorgestrel, which mainly stops or delays ovulation. If taken within 72hours of intercourse, it reduces the chance of pregnancy by about 85% in real‑world use. In Australia, most pharmacies sell it over‑the‑counter (OTC), so you don’t need a prescription.
Key attributes of the I‑Pill:
- Active ingredient: levonorgestrel
- Dosage: 1.5mg in a single tablet
- Window of effectiveness: up to 72hours (3days) after unprotected sex
- Typical cost in Australia: AUD30-40 per pack
- Side effects: nausea, fatigue, headache, mild spotting
Alternative #1 - Ulipristal Acetate (Ella)
Ulipristal acetate is a selective progesterone receptor modulator. It blocks the hormone’s action, preventing ovulation even later in the cycle than levonorgestrel can. In clinical trials, a single 30mg dose cut pregnancy risk by about 98% when taken within 120hours (5days).
In Australia, ulipristal acetate requires a prescription, but many pharmacists can dispense it after a brief telehealth consult. It’s marketed as Ella, though generic versions exist.
- Active ingredient: ulipristal acetate
- Dosage: 30mg single tablet
- Window of effectiveness: up to 120hours (5days)
- Typical cost: AUD80-100 per pack
- Side effects: headache, abdominal pain, menstrual changes
Alternative #2 - Copper Intrauterine Device (Paragard)
The copper IUD is the most effective form of EC known. Inserted by a trained clinician within 5days of intercourse, it releases copper ions that are toxic to sperm and prevent implantation. Its pregnancy‑prevention rate exceeds 99%.
Beyond emergency use, the copper IUD offers up to 10years of regular contraception, making it a dual‑purpose device for many.
Key details:
- Device name: Copper IUD (often sold as Paragard)
- Insertion window: within 120hours (5days)
- Cost of insertion (public sector): often covered by Medicare; private cost AUD200-300
- Side effects: cramping, heavier periods, occasional expulsion
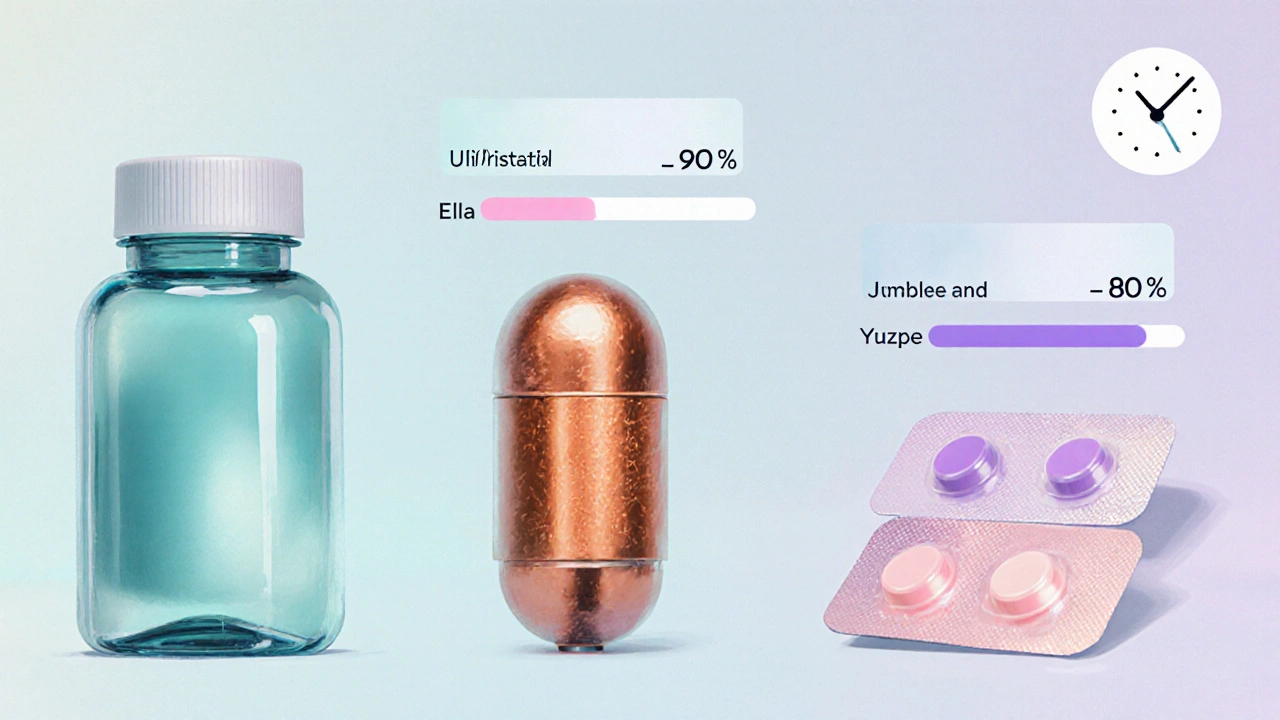
Alternative #3 - Yuzpe Method (Combined Oral Contraceptives)
The Yuzpe method uses high doses of estrogen and progestin found in regular birth‑control pills. Two doses are taken 12hours apart, ideally within 72hours of intercourse. Effectiveness is roughly 75%-85%, lower than dedicated EC pills.
Because the Yuzpe method relies on prescription‑only combined oral contraceptives (COCs), you need a doctor’s script or a pharmacist’s assessment.
- Active ingredients: estrogen (ethinylestradiol) + progestin (levonorgestrel or similar)
- Dosage: 2 tablets now, 2 tablets 12hours later
- Window of effectiveness: up to 72hours
- Side effects: nausea, vomiting, breast tenderness, menstrual spotting
Alternative #4 - Off‑Label Options (Mifepristone)
Mifepristone is a progesterone antagonist commonly used for medical abortion. Some clinicians prescribe a low dose (10mg) as EC up to 120hours after sex, citing studies that show comparable efficacy to ulipristal. It’s not listed on the PBS for EC, so access is limited to specialist clinics.
- Active ingredient: mifepristone
- Dosage: 10mg single tablet (off‑label)
- Window of effectiveness: up to 120hours
- Typical cost: AUD150-200 (private)
- Side effects: abdominal cramping, nausea, possible bleeding
Side‑by‑Side Comparison
| Attribute | I‑Pill (Levonorgestrel) | Ulipristal Acetate (Ella) | Copper IUD (Paragard) |
|---|---|---|---|
| Mechanism | Prevents/delays ovulation | Blocks progesterone receptors, stops ovulation later in cycle | Copper ions impair sperm, prevent implantation |
| Effective window | Up to 72hours | Up to 120hours | Up to 120hours |
| Typical efficacy | ~85% (real‑world) | ~98% (clinical) | >99% |
| Prescription needed? | No (OTC) | Yes (prescribed) | Yes (inserted by clinician) |
| Cost (AUD) | 30‑40 | 80‑100 | 200‑300 (private) or PBS‑covered |
| Common side effects | Nausea, headache, spotting | Headache, abdominal pain, menstrual shift | Cramping, heavier periods, rare expulsion |
How to Choose the Right Option for You
Deciding isn’t just about numbers; it’s about what fits your schedule, health profile, and budget. Here’s a quick decision matrix you can run in your head:
- Need it now and want no prescription? The I‑Pill is the simplest pick.
- Can wait a day or two, want the highest efficacy? Ulipristal or copper IUD are better.
- Prefer long‑term contraception after the emergency dose? The copper IUD gives up to a decade of protection.
- Have a history of hormonal sensitivity? The copper IUD avoids hormones entirely.
- Weighing cost? I‑Pill is cheapest OTC; copper IUD may be free under Medicare for eligible patients.

Practical Tips for Using Emergency Contraception Effectively
- Take it ASAP. Effectiveness drops sharply each hour after intercourse.
- Don’t double‑dose. One tablet of levonorgestrel or ulipristal is enough; extra pills won’t boost protection.
- Watch for vomiting. If you vomit within two hours of swallowing, repeat the dose with a new tablet.
- Follow up with a regular method. EC isn’t a replacement for ongoing birth control.
- Check interactions. Certain anti‑seizure meds, herbal supplements (e.g., St.John’s wort) can lower EC efficacy.
Potential Pitfalls and How to Avoid Them
Even the best‑studied drugs can backfire if used incorrectly. Common mistakes include:
- Waiting past the recommended window (especially risky with levonorgestrel).
- Assuming EC will terminate an existing pregnancy - it only works before implantation.
- Skipping a medical check after repeated EC use; frequent reliance may signal the need for a more reliable method.
- Overlooking weight considerations. Some data suggest levonorgestrel may be slightly less effective at body mass indexes over 30kg/m², making ulipristal a better fit.
Bottom Line: Tailor EC to Your Life
All four options have a place in Australia’s contraceptive toolkit. The I‑Pill’s convenience and low cost make it a solid default, but if you have a few extra hours, the higher efficacy of ulipristal or the near‑perfect protection of a copper IUD could be worth the extra step.
Remember, the most important thing is to act quickly and follow up with a regular birth‑control method that matches your routine. Emergency contraception is a safety net, not a long‑term solution.
Frequently Asked Questions
How soon after sex should I take the I‑Pill?
The sooner the better. Take it within the first 24hours for optimal protection; it still works up to 72hours but efficacy drops about 10% each day.
Can I use both levonorgestrel and ulipristal together?
No. Taking both can cause hormonal overload and side‑effects without improving efficacy. Choose one method based on timing and prescription availability.
Is the copper IUD safe for women who have never had a pelvic exam?
Insertion requires a brief pelvic exam to ensure the uterus is the right size and there are no infections. Most clinicians can perform it safely, even for first‑time users.
Do side effects from emergency contraception affect my next period?
Yes. Levonorgestrel may cause your next period to arrive a few days early or late, while ulipristal can shift the cycle by up to a week. The copper IUD may make bleeding heavier for the first few months.
Can I take emergency contraception if I’m breast‑feeding?
Levonorgestrel is generally considered safe for breastfeeding mothers, but ulipristal’s safety data are limited. Talk to your GP or pharmacist before choosing a method.



Aminat OT
October 13, 2025 AT 15:57I’m freaking out, I wish someone would just hand me an I‑Pill right now!
Amanda Turnbo
October 14, 2025 AT 19:44While the data presented is comprehensive, it’s worth noting that cost considerations often outweigh efficacy for many users.
In practice, the I‑Pill’s over‑the‑counter availability makes it a pragmatic first line.
However, the prescription barrier for ulipristal can be mitigated by telehealth services, which many clinics now offer.
Ultimately, personalized counseling remains essential.
Jenn Zuccolo
October 15, 2025 AT 23:31Choosing an emergency contraceptive can be viewed as a micro‑cosm of personal agency, a reminder that we sculpt our destinies in moments of urgency.
When the clock ticks, the I‑Pill offers immediacy, whereas ulipristal extends the safety net, embodying patience and foresight.
The copper IUD, on the other hand, transcends temporary measures, presenting a lasting covenant with one’s reproductive autonomy.
Therefore, the decision is less about hierarchy and more about alignment with one’s present circumstance and future aspirations.
Courtney The Explorer
October 17, 2025 AT 03:17From a pharmacodynamic standpoint, levonorgestrel‑based EC operates via HPO‑axis suppression-rapid, dose‑dependent, and temporally constrained!
Ulipristal, as a SPRM, introduces receptor antagonism that persists beyond the conventional 72‑hour window, thereby expanding the therapeutic index.
Meanwhile, the copper IUD leverages a physicochemical milieu-Cu²⁺ ionolysis-that impairs sperm motility and viability, achieving >99% efficacy.
Health systems must therefore implement tiered protocols integrating OTC accessibility with prescription‑driven pathways to optimize population‑level outcomes.
Ashleigh Connell
October 18, 2025 AT 07:04I love how this guide lays everything out in plain language-makes the whole EC maze feel like a walk in the park.
If you’re on a tight budget, the I‑Pill is still a solid safety net, and the copper IUD can be a game‑changer once you’re ready for a longer‑term solution.
Just remember to check any medication interactions, especially if you’re on anti‑seizure meds.
Erin Knight
October 19, 2025 AT 10:51Honestly, the author seems to gloss over the glaring socioeconomic disparity-slinging cheap I‑Pill options while casually mentioning “prescription‑only” methods as if they’re just a minor inconvenience.
The narrative lacks critical analysis of how pharmacy access points differ across urban and rural landscapes, thus betraying a superficial elitist viewpoint.
Kavita Jadhav
October 20, 2025 AT 14:37I hear you-it can feel overwhelming when you’re juggling cost, timing, and health concerns.
The I‑Pill is a reliable go‑to if you need something fast and affordable, but if you have a few extra hours, consider ulipristal for that extra peace of mind.
And don’t forget the copper IUD if you’re open to a longer‑term solution; many clinics now offer reduced fees for eligible patients.
Tony Halstead
October 21, 2025 AT 18:24Hey there! Let’s break this down step by step: first, assess how many hours have passed; second, weigh your budget; third, decide whether you prefer a hormonal or non‑hormonal option.
For most people, the I‑Pill is the quickest, but if you’re within 120 hours and can get a prescription, ulipristal adds a safety margin.
Remember, the copper IUD is not just emergency contraception-it doubles as a decade‑long birth control method, which can be a cost‑effective investment.
leo dwi putra
October 22, 2025 AT 22:11Picture this: the clock’s ticking, the panic rises, and you’re staring at a pharmacy shelf that looks like a warzone of pills and price tags. You reach for the I‑Pill, but then a voice whispers, “What if you could have a 99% guard against pregnancy for years?” That’s the drama of the copper IUD, a silent hero in the chaos.
Krista Evans
October 24, 2025 AT 01:57Exactly! You’ve got this moment of high stress, but you’re not alone-take a deep breath, remember that the I‑Pill is effective if you act quickly, and if you have a little extra time, ulipristal or the IUD are solid backup plans. You’ve got this!
Mike Gilmer2
October 25, 2025 AT 05:44Ah, the classic showdown: instant relief versus long‑term commitment-like choosing between a fireworks show and a sunrise that lasts a decade.
Alexia Rozendo
October 26, 2025 AT 08:31Sure, because nothing says “I’ve got my life together” like debating copper versus pills while waiting in line for coffee.
Kimberly Newell
October 27, 2025 AT 12:17Hey folks, just a quick heads‑up-if you’re looking for the I‑Pill, most pharmacies will have it on the shelf, no script needed. If you can’t find it, ask the pharmacist for “levonorgestrel emergency pill”-they’ll know what you need.
Drew Burgy
October 28, 2025 AT 16:04Obviously the government wants us to rely on “over‑the‑counter” meds so they can track our reproductive choices. Trust the shadow network of independent clinics for the real options like off‑label mifepristone.
Matt Laferty
October 29, 2025 AT 19:51When evaluating emergency contraception, it is essential to consider not only the pharmacological efficacy percentages but also the contextual variables that influence real‑world outcomes.
First, the temporal window of effectiveness directly correlates with the mechanism of action: levonorgestrel primarily prevents or delays ovulation, which becomes less reliable as follicular development progresses beyond the mid‑cycle.
Second, ulipristal’s selective progesterone receptor modulation confers a later point of intervention, thereby extending its efficacy to up to 120 hours, a factor that is especially pertinent for individuals who may experience delays accessing pharmacy services.
Third, the copper intrauterine device operates via a non‑hormonal pathway, introducing copper ions that impair sperm motility and viability, and for this reason it maintains a failure rate of less than 1% even when insertion occurs at the outer edge of the five‑day window.
From an economic perspective, the upfront cost of the I‑Pill (approximately AUD 30‑40) is modest, but when factoring in repeated use, cumulative expenses may surpass the one‑time insertion cost of a copper IUD, especially in health systems where the device is subsidised.
Additionally, patient preferences regarding hormonal exposure play a significant role; some women experience adverse reactions to levonorgestrel or ulipristal, such as nausea or menstrual irregularities, making the copper IUD an attractive hormone‑free alternative.
Healthcare providers should also be mindful of drug‑drug interactions-certain enzyme‑inducing anticonvulsants can reduce the plasma concentrations of both levonorgestrel and ulipristal, potentially diminishing their effectiveness.
Moreover, body mass index has been shown in some studies to modestly affect levonorgestrel efficacy, with higher BMI potentially necessitating the selection of ulipristal or the copper IUD for optimal protection.
Accessibility remains a critical barrier: while the I‑Pill is available over the counter in most Australian pharmacies, ulipristal requires a prescription, often obtainable through telehealth consultations, and the copper IUD necessitates a clinician‑performed insertion, which may not be feasible in remote areas.
Education campaigns that clearly articulate these nuances can empower individuals to make informed decisions aligned with their personal health goals.
In conclusion, no single emergency contraceptive method is universally superior; the optimal choice emerges from a synthesis of timing, cost, health status, and personal preference.
Clinicians and public health policymakers should strive to provide a diversified portfolio of options, ensuring that all individuals have equitable access to the method best suited to their circumstances.