Every year, over 3 million people worldwide get infected with hepatitis B or C. Most don’t know it until their liver is already damaged. The scary part? Both viruses are preventable or curable today-but millions still go undiagnosed and untreated. If you’ve ever wondered how these viruses spread, whether you should get tested, or if there’s real hope for a cure, here’s what actually matters right now.
How Hepatitis B and C Spread
Hepatitis B: More Contagious Than You Think
Hepatitis B isn’t spread by coughing, hugging, or sharing food. It’s spread by blood and bodily fluids. The most common way? From mother to baby during childbirth. In places like parts of Asia and Africa, up to 90% of chronic hepatitis B cases start this way. Even in low-risk countries, this is still a major source of infection. Sexual contact is another big one. If you’re unvaccinated and have sex with someone who has hepatitis B, your risk of catching it is 30% to 60%. That’s higher than HIV. Sharing needles-even once-is a direct route. The virus can live on a needle or razor for up to seven days. That’s why sharing personal items like toothbrushes or razors can be risky, especially in households where someone is infected. Healthcare workers are at risk too. A needlestick injury carries a 6% to 30% chance of transmission, depending on whether the source patient has high levels of the virus. It’s not common, but it happens.Hepatitis C: Blood-to-Blood Only
Hepatitis C is simpler in how it spreads: blood-to-blood contact. No other fluids matter. The biggest driver today? The opioid crisis. In the U.S., cases jumped 71% between 2014 and 2018. Most new infections are in people under 40 who inject drugs. Sharing needles, cookers, or cotton is the main cause. Mother-to-child transmission happens in about 5% to 6% of pregnancies. It’s rare but possible. Blood transfusions and organ transplants used to be a big risk-but since screening started in the early 1990s, that’s almost gone in developed countries. You won’t catch hepatitis C from a toilet seat, a handshake, or kissing. It doesn’t live in saliva or sweat. If you’ve never injected drugs, never had a tattoo with unsterile equipment, and never had a blood transfusion before 1992, your risk is extremely low.Who Should Get Tested
Hepatitis B Screening
The CDC now recommends everyone get tested for hepatitis B at least once in their life. But some groups need it more urgently:- Anyone born in regions with high hepatitis B rates (Asia, Africa, Eastern Europe, the Pacific Islands)
- Healthcare workers and first responders
- People who inject drugs
- Men who have sex with men
- People with HIV or other sexually transmitted infections
- Anyone about to start chemotherapy or kidney dialysis
- All pregnant women
Hepatitis C Screening
The CDC says every adult aged 18 and older should get one-time hepatitis C screening. Pregnant women need it too. That’s because many people have no symptoms for years-and by the time they feel sick, their liver is already damaged. High-risk groups should be tested regularly:- People who inject drugs (even once, years ago)
- People with HIV
- Those who got a blood transfusion or organ transplant before 1992
- People with abnormal liver enzyme levels
- Anyone born between 1945 and 1965 (baby boomers, who have the highest infection rates)
How Testing Works
Hepatitis B Testing
Hepatitis B isn’t checked with one test. It’s a panel:- HBsAg - If positive, you’re infected. This is the first sign.
- Anti-HBc - Shows you’ve been exposed to the virus, whether past or current.
- Anti-HBs - Means you’re protected, either from vaccination or past infection.
- HBeAg and HBV DNA - Used to see how active the virus is and whether treatment is needed.
Hepatitis C Testing
Hepatitis C testing is simpler:- Anti-HCV antibody test - First step. Positive means you’ve been exposed.
- HCV RNA test - If the antibody test is positive, this confirms if the virus is still active in your blood.
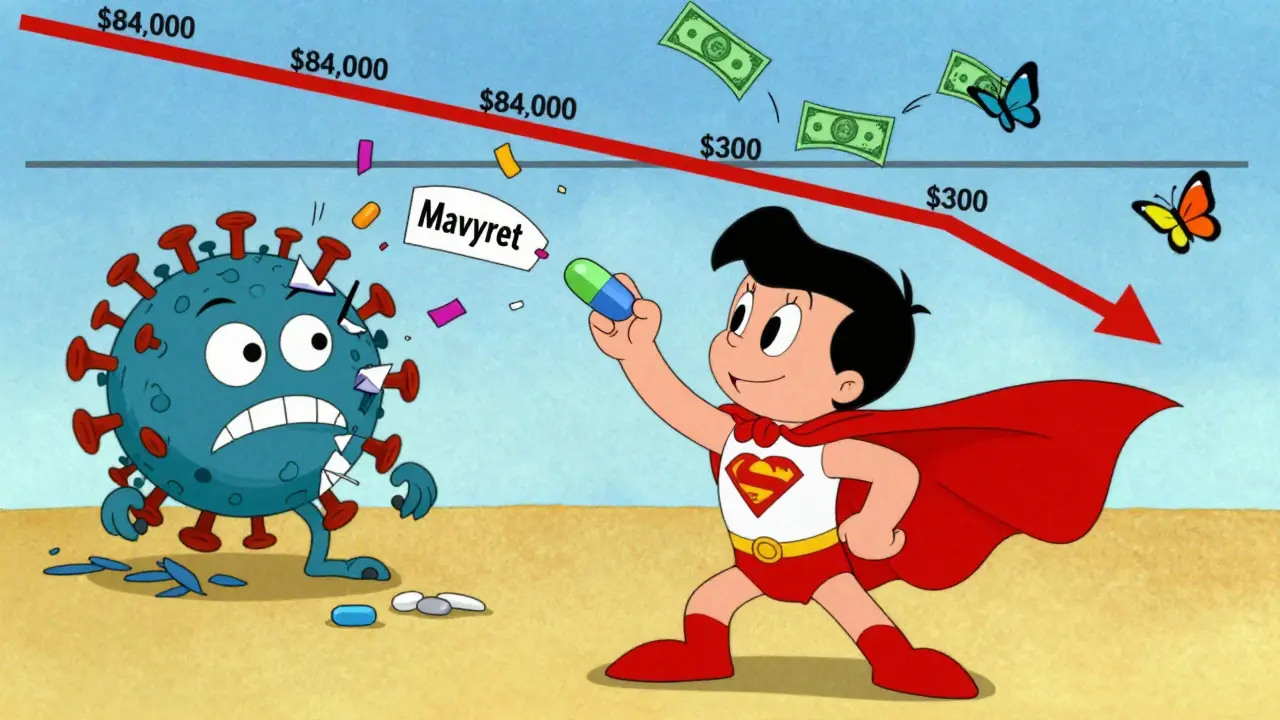
Treatment Advances: A Revolution in Hepatitis C
Hepatitis C used to be a life sentence. In the 1990s and early 2000s, treatment meant weekly injections of interferon for up to 48 weeks. Side effects were brutal: depression, fatigue, flu-like symptoms. Only about half of patients were cured. That changed in 2013 with the approval of sofosbuvir. Today, direct-acting antivirals (DAAs) like Epclusa and Mavyret cure over 95% of people in just 8 to 12 weeks. No injections. No hospital visits. Just pills. These drugs work by blocking the virus’s ability to copy itself. They’re so effective that even people with advanced liver disease or HIV co-infection can be cured. Side effects? Usually mild-headache or tiredness. The big win? Treatment is now available as generics for under $300 in countries like Egypt and India. In the U.S., prices dropped from $84,000 per course in 2014 to $24,000-$30,000 today. Many insurance plans cover it fully now. Egypt’s success story is proof it works. In 2008, 14.7% of Egyptians had hepatitis C. By 2021, after a national screening and treatment campaign, it dropped to 0.9%. That’s 10 million people treated. It’s not science fiction-it’s real.Hepatitis B: No Cure Yet, But Better Control
Unlike hepatitis C, there’s no cure for hepatitis B. But we can control it extremely well. The go-to drugs are tenofovir alafenamide (TAF) and entecavir. They stop the virus from multiplying. They’re taken as one pill a day. Side effects are rare. They’re so safe, even pregnant women can take them. These drugs don’t eliminate the virus. They suppress it. So you usually need to take them for life. But that’s enough. People on treatment have a near-normal life expectancy. Their risk of liver cancer and cirrhosis drops by over 80%. A new hope? Functional cure. That means losing the hepatitis B surface antigen (HBsAg) from your blood. It’s rare-only 1% to 2% of people achieve this naturally each year. But new drugs are in trials:- siRNA drugs like JNJ-3989 silence the virus’s genetic material.
- Capsid modulators disrupt how the virus builds its shell.
- Therapeutic vaccines try to train your immune system to fight the virus.
Barriers to Getting Help
We have the tools. But we’re not using them. Only 21% of people with hepatitis C in the U.S. got treated in 2020. Why? Cost, stigma, and lack of awareness. Many people think they’re not at risk. Others fear judgment if they admit to drug use. For hepatitis B, vaccine coverage in U.S. adults is just 66.5%. The goal is 90%. Birth-dose vaccination (given within 24 hours of birth) is still not universal in many countries. That’s why hepatitis B stays endemic. In rural areas and among people who inject drugs, testing and treatment access is still poor. Mobile clinics and community health workers are filling the gap. In Australia, outreach programs in prisons and drug treatment centers have boosted testing by over 50% in five years.What You Can Do Today
If you’re reading this, here’s your action plan:- Get tested for both hepatitis B and C. One blood test can tell you everything.
- If you’re negative for hepatitis B and not immune, get vaccinated. Three shots over six months give lifelong protection.
- If you have hepatitis C, talk to your doctor about DAAs. You can be cured.
- If you have chronic hepatitis B, see a liver specialist. Don’t wait for symptoms.
- If you use drugs, never share needles. Use clean equipment. Needle exchange programs save lives.


Matt Davies
December 19, 2025 AT 00:11Man, I never realized how much of a game-changer those hepatitis C pills are. I had a cousin who went through the old interferon hell-cried every week, lost 30 pounds, couldn’t work. Now? Just swallow a few pills and boom, virus gone. It’s like magic if you think about it. The fact that Egypt cured 10 million people? That’s not just medicine, that’s a revolution.
holly Sinclair
December 19, 2025 AT 16:13It’s fascinating how the biology of these viruses reveals so much about societal neglect. Hepatitis B persists not because we lack tools, but because we treat it as a moral failure rather than a public health issue. The mother-to-child transmission rate in high-prevalence regions isn’t just a medical statistic-it’s the consequence of decades of underfunded maternal care, colonial legacies in healthcare infrastructure, and the quiet abandonment of populations deemed ‘low priority.’ We cure hepatitis C with pills but still let babies inherit hepatitis B because we don’t prioritize birth-dose vaccines in poor communities. That’s not science. That’s ethics in reverse.
Emily P
December 19, 2025 AT 18:52I got tested last year after reading this kind of thing. Negative for both. Got the HB vaccine right away. Feels good to know I’m not a walking time bomb.
Andrew Kelly
December 21, 2025 AT 01:58Let me guess-the CDC wants you to get tested because they’re paid by Big Pharma. You think these ‘cures’ are real? The liver doesn’t just heal from a pill. They’re hiding the truth: these drugs cause long-term immune damage, and the real cure is fasting and alkaline diets. I’ve been off meds for 12 years and my liver enzymes are perfect. They don’t want you to know that.
Anna Sedervay
December 21, 2025 AT 18:58While I appreciate the clinical precision of this exposition, I must respectfully contend that the omission of epigenetic transgenerational susceptibility factors in hepatitis B persistence constitutes a glaring lacuna in the current discourse. One cannot, in good conscience, reduce a complex immunovirological phenomenon to mere ‘pill-taking’ without acknowledging the ontological weight of ancestral trauma and its modulation of hepatic gene expression. The WHO targets are laudable, yet fundamentally reductive.
Jedidiah Massey
December 23, 2025 AT 15:49DAAs? More like DAA-sssss (Direct-Acting Antivirals, obviously). 😎 The cost drop from $84k to $24k? Still a ripoff. My cousin in India paid $200 for a 12-week course. Meanwhile, my insurance in the US made me jump through 17 hoops just to get pre-auth. Pharma’s still playing us. #PharmaScam
bhushan telavane
December 25, 2025 AT 04:22In India, we used to see so many people with jaundice. Now, even small clinics give free tests. My uncle got treated for Hep C last year-no hospital stay, just pills. The government even sent a team to our village. It’s not perfect, but it’s changing. We need more of this.
Mahammad Muradov
December 27, 2025 AT 01:51You people talk about testing like it’s a miracle. But if you don’t have clean water, proper sanitation, or education on hygiene, testing is just a placebo. People in rural India still share razors because they can’t afford their own. No pill fixes poverty. Stop pretending medicine alone can solve this.
Alex Curran
December 28, 2025 AT 19:16Functional cure for HBV by 2030 sounds optimistic but plausible. The siRNA and capsid modulators are the real deal. I’ve seen phase 2 data-HBsAg seroclearance hitting 15% in some cohorts. That’s massive. We’re not talking about suppression anymore. We’re talking about immune reconstitution. This isn’t just progress. It’s a paradigm shift.
Lynsey Tyson
December 29, 2025 AT 19:32I just want to say thank you for writing this. I used to be scared to even ask my doctor about testing because I thought they’d judge me. But reading this made me feel like it’s okay to care about my health without shame. I’m getting tested next week.