When you buy a hearing aid, you’re not just buying a device-you’re buying better hearing. But here’s the truth most people don’t know: real-ear measurement isn’t just a nice-to-have step in fitting. It’s the only way to make sure the device actually works for your ears.
What Real-Ear Measurement Really Does
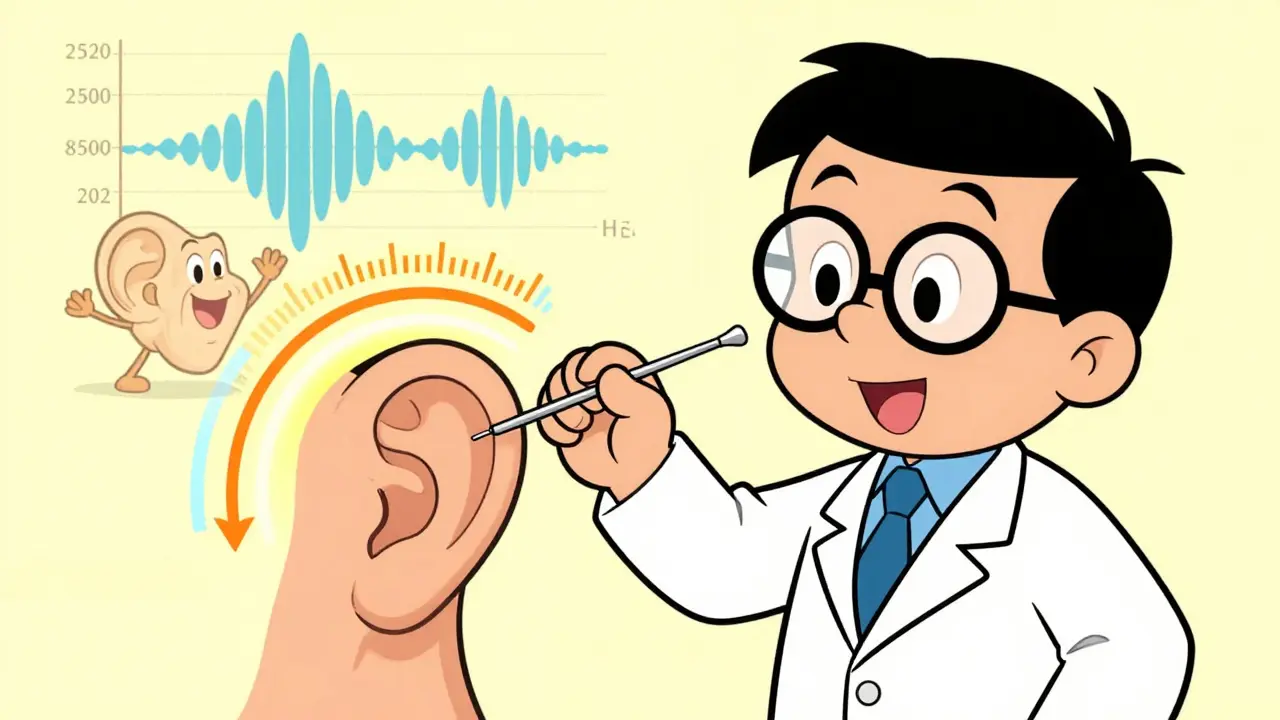
Real-ear measurement (REM) is a scientific process that checks exactly how much sound your hearing aid delivers inside your ear canal. It’s not a guess. It’s not a simulation. It’s a direct measurement using a tiny microphone placed near your eardrum while you’re wearing the hearing aid. Think of it like this: every ear is different. The shape, length, and curvature of your ear canal change how sound travels. Two people with the same hearing loss can get the same hearing aid model, but if one has a longer, narrower canal, that device might deliver 15 dB less volume than intended. That’s the difference between hearing clearly and still struggling in a crowded room. REM fixes that. It measures sound pressure levels across frequencies-from low rumbles at 250 Hz to high-pitched speech sounds at 8000 Hz-with precision within ±2 dB, as required by ANSI standards. The system compares what’s actually coming out of your hearing aid to a target curve based on your specific hearing loss and the prescriptive formula your audiologist uses-like NAL-NL2 or DSL v5.0. If the output doesn’t match, the device is adjusted until it does.Why Manufacturer Settings Alone Don’t Work
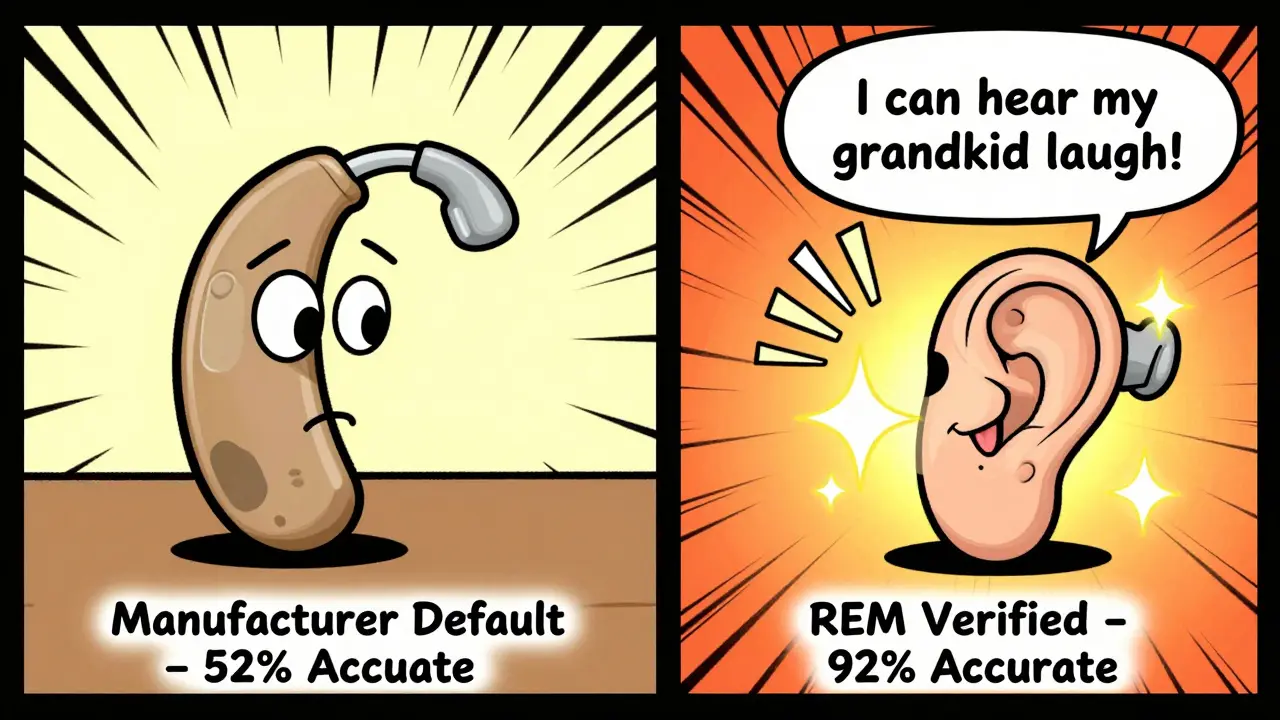
Most hearing aids come with a “first fit” setting. That’s the default program the manufacturer suggests based on your audiogram. It’s a starting point. But studies show it’s only about 52% accurate at matching real-world needs. Why? Because those settings are based on average ear canal sizes. They assume your ear looks like a standard 2cc coupler used in labs. But real ears aren’t lab models. Research from the International Journal of Audiology found ear canal resonance can vary by up to 20 dB between individuals. That’s massive. If your ear naturally amplifies high frequencies, a hearing aid set for an “average” ear will over-amplify them-making voices sound sharp, tinny, or even painful. Even the best software simulations from companies like Oticon or Phonak only predict real-ear performance with 65% accuracy. REM doesn’t predict-it measures. And when it does, accuracy jumps to 92%.The Real-World Impact on Your Hearing
The difference isn’t theoretical. A 2019 study in the Journal of the American Academy of Audiology found patients who had REM during fitting understood speech in noisy environments 35% better than those who didn’t. Survey data from HealthyHearing.com in 2022 showed 87% of users who had REM rated their hearing aids as “very effective.” Among those without REM, that number dropped to 52%. Reddit users in r/hearingloss consistently report the same: “The REM process was slightly uncomfortable, but knowing my aids were precisely calibrated made all the difference.” People who skip REM often end up with complaints: “It’s too loud,” “My voice sounds weird,” “It whistles when I eat.” These aren’t just annoyances-they’re signs the device isn’t matched to your ear. And they lead to frustration, abandonment, and lost quality of life.How the Process Actually Works
The REM procedure is quick, non-invasive, and done right in the clinic. Here’s what happens:- Your audiologist checks your ear canal with an otoscope to make sure there’s no wax buildup, infection, or perforation.
- A thin probe tube (about 0.5-1.0 mm wide) is gently inserted into your ear canal, positioned within 5 mm of your eardrum. This is measured from the intertragal notch.
- Your hearing aid is inserted while keeping the probe tube in place.
- A calibrated speaker plays speech sounds at different volumes-typically 50 dB (quiet), 65 dB (normal conversation), and 80 dB (loud).
- The probe microphone records the actual sound pressure at your eardrum and compares it to your target curve.
- The audiologist adjusts the hearing aid settings until the output matches the target across all frequencies.
What Happens Without REM
Skip REM, and you’re relying on guesswork. That’s what most over-the-counter (OTC) hearing aids do. The FDA’s 2022 OTC Hearing Aid Rule explicitly states these devices “cannot replace the need for professional evaluation and fitting.” Why? Because they have no way to verify output in your unique ear. Even among professionals, the gap is wide. According to the Hearing Industries Association’s 2022 survey, 97% of audiologists use REM routinely. But only 12% of retail hearing aid specialists (non-audiologists) do. That means if you buy a hearing aid at a big-box store or online without seeing a certified audiologist, you’re almost certainly getting an unverified fit. The result? More returns. More adjustments. More wasted time and money.Why REM Saves You Money in the Long Run
Some people think REM adds cost. It doesn’t. It saves you money. A 2021 study in the International Journal of Audiology found patients who had REM needed 43% fewer follow-up visits for adjustments. Why? Because the hearing aid was right the first time. Medicare and most private insurers cover REM under CPT code 92597. That’s because the American Medical Association recognizes it as a medical necessity-not a luxury. If you’re paying out of pocket, think of it this way: spending $100-$150 on REM avoids $500-$1,000 in replacement costs, repeated fittings, or buying a second device because the first one didn’t work.Common Concerns and Myths
Some people worry the probe tube will hurt. The truth? About 22% of first-time patients feel a mild tickling sensation. Only 2% report discomfort beyond that. And 98% say it’s brief and totally tolerable. Others think 3D ear scans or AI tools will replace REM. Not anytime soon. A 2023 study in Ear and Hearing showed 3D scans can help with custom earmolds, but they can’t measure real-ear sound pressure. Dr. Pamela Souza put it plainly in her 2022 AAA keynote: “No matter how advanced our modeling becomes, we’ll always need to verify what’s actually happening in the real ear.” And yes, REM takes time. But so does getting your car’s alignment wrong and having to fix it three times.
What to Ask Your Audiologist
Before your fitting, ask these questions:- Will you use real-ear measurement to verify my hearing aid settings?
- What prescriptive target are you using (NAL-NL2, DSL v5.0, etc.)?
- Can I see the real-ear gain curves before and after adjustment?
- Will you test at multiple input levels (50, 65, and 80 dB)?
- Do you document the results in my chart?
The Future of Hearing Aid Verification
REM isn’t standing still. New tools are emerging. Widex’s 2023 MOMENT 2 platform uses AI to analyze REM data faster, cutting fitting time by 30%. The International Organization for Standardization now requires REM verification for all hearing aids sold in Europe. And the NIH is funding $2.4 million in research to make REM even more efficient. But the core hasn’t changed. The goal is still the same: make sure what’s programmed into the device matches what’s actually reaching your cochlea. Because hearing isn’t about numbers on a screen. It’s about understanding your child’s laugh, your partner’s voice, the sound of rain on the roof.Final Thought
Hearing aids aren’t like glasses. You can’t just pick a strength and call it done. Your ears are complex, unique, and full of acoustic surprises. Real-ear measurement is the only tool that cuts through the guesswork. It’s the difference between hearing and truly listening. If you’re getting a hearing aid, demand REM. Don’t settle for anything less.Is real-ear measurement painful?
No, it’s not painful. A thin probe tube is gently placed in your ear canal, about 5 mm from your eardrum. Most people feel a slight tickling sensation, especially during insertion. About 22% of first-time users report mild discomfort, but 98% say it’s brief and tolerable. It’s nothing like a dental exam or ear cleaning. The process is quick, and you’re awake and in control the whole time.
Can I skip REM if I’m using over-the-counter (OTC) hearing aids?
The FDA explicitly warns that OTC hearing aids cannot replace professional evaluation and fitting. These devices are designed for mild hearing loss and come with no verification. Without REM, you’re relying on generic settings that may not match your ear’s acoustics. Many users report whistling, distorted sound, or lack of clarity-problems that disappear with professional verification. If you have moderate or severe hearing loss, OTC aids are not a substitute for a full audiological evaluation and REM.
Why do some audiologists skip REM?
Some audiologists skip REM due to time pressure, lack of equipment, or insufficient training. But according to the American Academy of Audiology, REM is the gold standard and should be used for every fitting. Retail hearing aid specialists-who are not required to be audiologists-are far less likely to use it. If your provider doesn’t offer REM, ask why. If they can’t explain, consider finding someone who does. Your hearing is worth the extra step.
Does REM work for children and babies?
Yes, and it’s even more critical for children. The 2023 Joint Committee on Infant Hearing states REM is essential for all pediatric fittings. Kids’ ear canals are smaller and change rapidly as they grow. Standard coupler measurements are useless here. REM ensures the hearing aid delivers the right amount of sound at every frequency, which is vital for speech and language development. Specialized probe tubes and techniques are used for infants and young children to ensure safety and accuracy.
Is REM covered by insurance?
Yes, in most cases. Medicare and most private insurers cover REM under CPT code 92597. The American Medical Association recognizes it as a medical necessity for hearing aid fittings. If your provider says it’s not covered, ask them to submit the code. If they refuse to use it, that’s a red flag. You’re paying for a service that’s medically recognized-and you should get it.
How do I know if my audiologist is doing REM correctly?
Ask to see the real-ear gain curves before and after adjustment. A good audiologist will show you the target curve (based on your hearing loss) and the actual measured output. They should test at multiple input levels (50, 65, and 80 dB) and explain why changes were made. They should also document the results in your chart. If they just say “it’s set” without showing you data, they’re not following best practices.
Can REM be done with Bluetooth or wireless hearing aids?
Yes. Modern REM systems can measure output even when the hearing aid is streaming audio via Bluetooth. The probe microphone measures the actual sound reaching your eardrum regardless of how the signal is delivered. Some systems even allow testing with live speech or music input. The key is that the measurement happens inside your ear canal, not in a test box or through software simulation.
What if my hearing changes after the fitting?
Hearing can change over time-especially with age or noise exposure. If you notice your hearing aid isn’t working as well as it used to, schedule a re-evaluation. Your audiologist should repeat REM to check if the settings still match your current hearing loss. Don’t wait until you’re struggling. A quick verification check can restore clarity without needing a new device.


Dan Nichols
January 26, 2026 AT 11:08Let me get this straight - you’re telling me I need to pay extra just to make sure my hearing aid doesn’t sound like a tin can full of wasps? And this is standard practice? I’ve had mine for two years and never once had this done. My wife says I still yell at the TV, but hey, at least I didn’t waste $150 on a tube up my ear.
Renia Pyles
January 26, 2026 AT 15:43Oh please. This whole REM thing is just audiologists’ way of padding their bills. I got my OTC hearing aids off Amazon for $300, tweaked the bass in the app, and now I can hear my cat sneeze from the other room. Who needs a microphone in their ear canal when you’ve got AI and a decent smartphone? You’re being manipulated by the medical-industrial complex.
Rakesh Kakkad
January 27, 2026 AT 19:41Respected colleagues, I write from New Delhi where hearing care remains a luxury. In our public hospitals, we rarely possess REM equipment. Yet, we fit hearing aids daily - guided by experience, patient feedback, and prayer. The science you describe is elegant, yes, but not accessible to millions. Is the gold standard truly ethical when it excludes the poor?
Nicholas Miter
January 28, 2026 AT 16:13I had REM done last year. Honestly? It was weird. That little tube felt like a bug crawling in there. But after they adjusted it? My kid’s voice didn’t sound like she was talking through a cardboard tube anymore. I didn’t even know I was missing the high notes in her laugh. That’s the thing - you don’t miss what you never heard. It’s not about the tech. It’s about the moments.
George Rahn
January 29, 2026 AT 13:25Let us not mince words - this is not merely audiological science. This is the triumph of empirical verification over the pathetic, neoliberal delusion that mass-market devices can replace human expertise. The American ear is not a widget. It is not a commodity to be optimized by algorithmic guesswork. REM is the last bastion of medical integrity in a world where everything is outsourced to Silicon Valley and sold on TikTok. If you skip REM, you are not just poorly fitted - you are culturally complicit in the erosion of care.
Ashley Karanja
January 31, 2026 AT 09:59As someone who’s been navigating hearing loss for over a decade - and who’s sat through more fittings than I can count - I can say with absolute certainty that REM is the difference between auditory fatigue and auditory peace. The prescriptive targets (NAL-NL2, DSL v5.0) aren’t arbitrary; they’re evidence-based, calibrated to the spectral sensitivity of human speech perception. When the output curve aligns with your individual audiogram and your ear canal’s acoustic impedance - which varies wildly even between left and right ears - you’re not just hearing better, you’re cognitively conserving energy. The brain stops straining. The stress drops. The quality of life metrics? They spike. And no, AI simulations or 3D scans can’t replicate that. The ear is a living resonator, not a circuit board.
Karen Droege
February 1, 2026 AT 06:15I work in a clinic in Vancouver and I’ve seen it all. People come in with OTC devices that whistle like a kettle, or make their own voice sound like a robot in a haunted house. One guy cried because he hadn’t heard his granddaughter say ‘I love you’ clearly in three years - until we did REM. We adjusted the high-frequency gain by 8 dB, and he just sat there, silent, for a full minute. Then he whispered, ‘I didn’t know I was missing that.’ That’s not a procedure. That’s a miracle. If your provider won’t do REM, find someone who will. Your ears are not disposable.
Robin Van Emous
February 3, 2026 AT 02:22Thanks for sharing this. I didn’t know REM was covered by insurance. I’ve been putting off getting new aids because I thought it was too expensive. But now I’m calling my audiologist tomorrow. I just want to hear my wife’s voice without asking her to repeat everything. That’s all.
Angie Thompson
February 3, 2026 AT 17:14My grandma got her first hearing aid last year - and they did REM. She said it felt like magic. Now she can hear birds outside her window again. I cried. You’re not just fixing a device. You’re restoring wonder. 🌿👂❤️