Hashimoto’s thyroiditis is the most common reason people end up with an underactive thyroid. It’s not just a simple hormone problem-it’s your immune system turning against your own thyroid gland. Over time, this attack slowly destroys the gland’s ability to make thyroid hormone, leading to hypothyroidism. If you’ve been told you have Hashimoto’s, you’re not alone. About 4% of adults in the U.S. have it, and women are five to ten times more likely to be affected than men. The good news? It’s manageable. The key is understanding how TSH monitoring guides your treatment-and why it’s the most important tool you have.
How Hashimoto’s Turns Your Immune System Against Your Thyroid
Your thyroid is a small butterfly-shaped gland at the base of your neck. It makes hormones that control your metabolism, energy, mood, and body temperature. In Hashimoto’s, your immune system mistakenly sees thyroid tissue as a threat. It produces antibodies-mainly thyroid peroxidase antibodies (TPOAb)-that attack the gland. This inflammation doesn’t happen overnight. It can take years before your thyroid can’t keep up with demand.That’s why many people feel fine at first. You might have fatigue, weight gain, or brain fog for months or even years before your doctor spots a problem. The first clue is often a high TSH level. TSH, or thyroid-stimulating hormone, is made by your pituitary gland. When your thyroid isn’t producing enough hormone, your pituitary pushes harder-raising TSH to try to wake it up. A TSH above 4.5 mIU/L is usually the red flag that starts the diagnostic process.
Once TSH is high, doctors check two things: free T4 (the active thyroid hormone in your blood) and TPOAb. If T4 is low or low-normal and TPOAb is elevated (usually over 35 IU/mL), the diagnosis is clear. You have Hashimoto’s. And here’s the critical part: once you’re diagnosed, you don’t need to keep testing those antibodies again. The ATA and Cleveland Clinic both say antibody levels don’t tell you if your treatment is working. Only TSH does.
Why TSH Is the Only Test That Matters for Treatment
You might think checking your T4 or T3 levels would give you a better picture. But in Hashimoto’s, that’s not the case. Multiple guidelines-from the American Thyroid Association to the Royal Australian College of General Practitioners-agree: for people with primary hypothyroidism (which includes Hashimoto’s), TSH is the only test you need to monitor treatment.Why? Because your pituitary gland is exquisitely sensitive to thyroid hormone levels. Even tiny changes in T4 cause big shifts in TSH. That makes TSH a precise, early warning system. If your levothyroxine dose is too low, TSH rises. Too high? TSH drops. That’s why doctors don’t routinely check T4 or T3 after diagnosis. Doing so adds cost and confusion without improving outcomes.
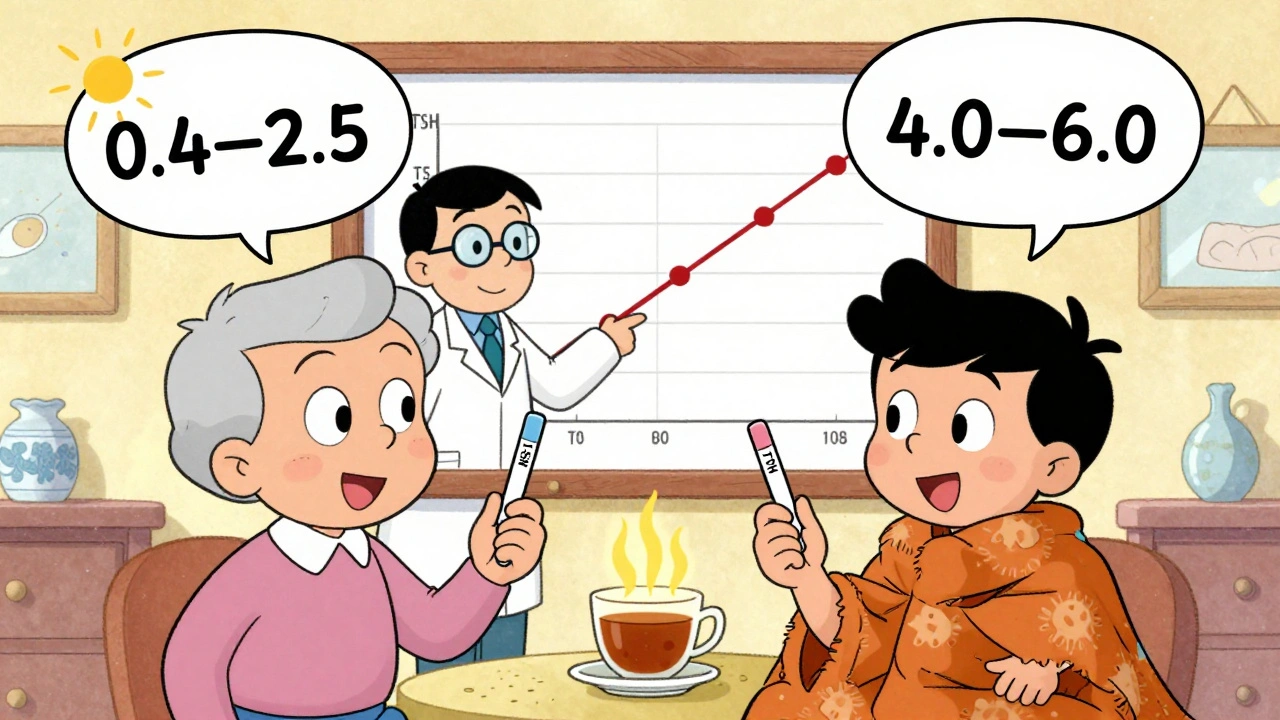
The target TSH range for most adults under 65 is 0.4 to 4.0 mIU/L. But that’s not one-size-fits-all. Some people feel their best when their TSH is closer to 1.0 or 1.5. Others do fine with a TSH near 3.5. Your doctor will start with the standard range, but your symptoms matter too. If you’re still tired, cold, or depressed despite a TSH in range, your doctor might try lowering it to 0.4-2.5 mIU/L. That’s not a mistake-it’s personalized care.
For people over 65, slightly higher TSH levels (up to 6.0 mIU/L) are often acceptable. Older adults are more sensitive to the side effects of too much thyroid hormone, like heart rhythm problems or bone loss. So the goal shifts from perfect normalization to safe, symptom-free function.
Levothyroxine: The Standard Treatment and How Dosing Works
Levothyroxine (LT4) is the only medication you’ll need. It’s a synthetic version of T4, the hormone your thyroid should be making. Brands like Synthroid and Levoxyl are common, but most people take generic levothyroxine-it’s just as effective and far cheaper. The FDA tightened manufacturing rules in 2018 to make sure every pill has the same potency, which was a big win for patients who used to have TSH swings from switching brands.Dosing starts at about 1.4 to 1.8 mcg per kilogram of body weight. For most adults, that’s 50 to 75 mcg per day. But if you’re older, have heart disease, or have mild hypothyroidism (subclinical), doctors often start lower-25 to 50 mcg. Why? Because going too fast can cause palpitations, anxiety, or even a heart attack in vulnerable people.
It takes time for your body to adjust. Levothyroxine has a long half-life-it stays in your system for weeks. That’s why you can’t just change your dose every week. You need to wait 6 to 8 weeks after a dose change before retesting TSH. This gives your pituitary time to respond. Many patients get frustrated: “I feel awful, and I have to wait two months to adjust?” But rushing leads to overshooting. And once you’re over-replaced, it’s harder to bring TSH back down.
Adjustments are usually made in 12.5 to 25 mcg increments. If your TSH is 7.0 and you’re on 50 mcg, your doctor might bump you to 75 mcg. Wait 6-8 weeks. Retest. If TSH is now 3.0 and you still feel tired, maybe go to 87.5 mcg. It’s a slow dance. Don’t expect to find your perfect dose in one try. Most people need two to four adjustments before they’re stable.

When and How Often to Test TSH
Timing matters. Test too soon, and you’ll get a misleading number. Wait too long, and you’re stuck with symptoms.After starting levothyroxine, your first TSH test should be 6 to 8 weeks later. Same after any dose change. Once you’re stable-meaning your TSH has stayed in range for at least three months-you can switch to annual testing. Some guidelines, like the RACGP, suggest checking every 6 months at first, then yearly. If you’re pregnant, it’s different. You’ll need testing every 4 weeks until week 20 of pregnancy, because your body’s demand for thyroid hormone increases dramatically. Untreated or poorly managed Hashimoto’s during pregnancy raises the risk of miscarriage, preterm birth, and developmental issues in the baby.
Other situations call for more frequent checks:
- You start or stop estrogen (birth control pills, hormone therapy)
- You begin or stop iron, calcium, or proton pump inhibitors (like omeprazole)
- Your weight changes by more than 10%
- You switch levothyroxine brands (even generics-batch differences can still happen)
- You develop new symptoms like rapid heartbeat, unexplained weight loss, or insomnia
Don’t assume your TSH is fine just because you’re on medication. Many people are under-treated because they don’t get tested regularly. A 2022 study by Quest Diagnostics showed over 15 million TSH tests were done in the U.S. that year-proof of how common and ongoing this management is.
What Your Symptoms Tell You (Even When TSH Looks Good)
TSH is the guide, but your body is the final judge. If your TSH is in range but you still feel exhausted, constipated, or depressed, something’s off. You might need a lower target. If you’re anxious, losing weight without trying, or having trouble sleeping, your dose might be too high.These symptoms aren’t “all in your head.” They’re real signals from your metabolism. Fatigue and cold intolerance mean your thyroid hormone is too low. Heart racing, tremors, or insomnia mean it’s too high. Don’t ignore them just because your lab report says “normal.”
Some patients find that keeping a simple symptom journal helps. Note your energy levels, mood, weight, sleep, and bowel habits each week. Bring it to your appointment. It gives your doctor context beyond numbers.
There’s also growing evidence that genetics play a role. A 2023 study in JAMA Internal Medicine found that people with a certain DIO2 gene variant respond better to TSH targets in the lower half of the normal range (0.4-2.0 mIU/L). That’s not routine testing yet-but it’s a sign that personalized treatment is coming.
What Doesn’t Work-and What’s Still Being Studied
You might hear about “natural” thyroid treatments, desiccated pig thyroid (Armour Thyroid), or T3/T4 combo pills. The American Thyroid Association and Cochrane Review both say there’s no strong evidence these are better than levothyroxine alone. In fact, T3 can cause dangerous spikes in heart rate and is harder to control. Most endocrinologists stick with LT4 because it’s stable, predictable, and safe.Home TSH tests like ThyroChek were approved by the FDA in 2021. But they’re not yet recommended for routine use. They’re less accurate at low TSH levels, and if you’re on medication, even small errors can lead to wrong dose changes. Stick with lab tests until guidelines change.
Research is ongoing into whether diet, stress, or gut health affects Hashimoto’s progression. While some patients report feeling better on gluten-free diets, no large studies prove it stops the autoimmune attack. Focus on what works: consistent levothyroxine, regular TSH checks, and listening to your body.
Living Well With Hashimoto’s
Hashimoto’s isn’t a death sentence. It’s a chronic condition that, with the right care, lets you live a full, normal life. The biggest mistake people make is thinking they’re “cured” once they start medication. You’re not. You’re managing. And that means staying on top of your TSH.Take your pill the same way every day-on an empty stomach, 30 to 60 minutes before breakfast. Avoid calcium, iron, or soy within 4 hours. These interfere with absorption. Keep your dose consistent. Don’t skip days. And never stop without talking to your doctor.
Most people find their sweet spot within a year. You’ll have more energy. Your weight will stabilize. Your brain fog lifts. But it takes patience. The system is slow. The science is clear. And you’re not alone.
Can Hashimoto’s thyroiditis be cured?
No, Hashimoto’s thyroiditis cannot be cured. The autoimmune attack on the thyroid gland is permanent. However, the resulting hypothyroidism can be fully managed with daily levothyroxine medication. Once the right dose is found, most people experience no symptoms and live normal, healthy lives. Treatment doesn’t stop the immune system from attacking-it replaces the hormone the thyroid can no longer make.
Why do I need to keep checking TSH if I feel fine?
Even if you feel fine, your body’s needs can change. Weight gain or loss, aging, pregnancy, new medications, or even seasonal changes can affect how much thyroid hormone you need. TSH is the most sensitive indicator of whether your dose is still right. Skipping tests can lead to under- or over-treatment, which causes symptoms you might not even connect to your thyroid. Annual checks are the minimum-more often if your situation changes.
Is it safe to take levothyroxine long-term?
Yes. Levothyroxine is a synthetic version of the hormone your body naturally makes. When taken at the correct dose, it’s one of the safest medications available. Long-term use doesn’t damage your organs or cause dependency. The only risk comes from taking too much, which can lead to bone loss or heart rhythm problems. That’s why regular TSH monitoring is essential-it keeps your dose precise and safe.
Do thyroid antibodies need to be checked regularly?
No. Once Hashimoto’s is diagnosed by elevated TPOAb levels, repeating antibody tests offers no benefit for treatment. Antibody levels don’t correlate with symptoms or how well your medication is working. The American Thyroid Association explicitly states that monitoring antibody titers is unnecessary. Your TSH level is the only test that matters for managing your condition.
Can diet or supplements cure Hashimoto’s?
No. While some people report feeling better on gluten-free, dairy-free, or anti-inflammatory diets, there’s no scientific proof these diets stop the autoimmune process or reduce antibody levels. Supplements like selenium may slightly lower antibodies in some studies, but they don’t replace thyroid hormone. Levothyroxine remains the only proven treatment. Focusing on diet alone can delay proper care and lead to worsening symptoms.
What happens if I miss a dose of levothyroxine?
Missing one dose won’t cause immediate problems. Levothyroxine has a long half-life, so your body still has enough hormone in reserve. If you miss a dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Then skip the missed one and return to your regular schedule. Don’t double up. Consistency matters more than perfection. But if you’re regularly missing doses, talk to your doctor. Poor adherence is one of the top reasons people have persistent symptoms despite being on medication.
If you’re managing Hashimoto’s, you’re doing something most people never have to think about: fine-tuning your body’s core metabolism. It’s not glamorous. But it’s powerful. With the right TSH monitoring and consistent medication, you can feel like yourself again-energized, clear-headed, and in control.

Saurabh Tiwari
December 2, 2025 AT 14:36Sandi Allen
December 3, 2025 AT 02:00John Morrow
December 3, 2025 AT 12:32ruiqing Jane
December 4, 2025 AT 11:47Michael Campbell
December 5, 2025 AT 07:57Victoria Graci
December 6, 2025 AT 11:23Saravanan Sathyanandha
December 6, 2025 AT 15:37alaa ismail
December 8, 2025 AT 03:39Fern Marder
December 8, 2025 AT 14:04Carolyn Woodard
December 9, 2025 AT 09:19Kristen Yates
December 10, 2025 AT 03:27Allan maniero
December 10, 2025 AT 06:31