Diuretic Selection Tool
This tool helps you understand which diuretic might be most appropriate for your specific situation. Based on your responses, you'll receive personalized recommendations with explanations. This is not a substitute for medical advice, but a tool to help you better discuss options with your doctor.
What to discuss with your doctor
Your doctor will consider all your factors when choosing a diuretic. Important considerations include:
- • Kidney function and electrolyte balance
- • Other medications you take
- • Your specific symptoms and severity
- • Cost and insurance coverage
- • Your lifestyle and ability to take medications
When your body holds onto too much fluid, it can make you swell, feel short of breath, or raise your blood pressure. Furosemide has been the go-to pill for this for decades. But is it still the best choice? Many people are asking: are there better, safer, or more effective alternatives? The answer isn’t simple. It depends on your condition, your other meds, your kidneys, and even your diet.
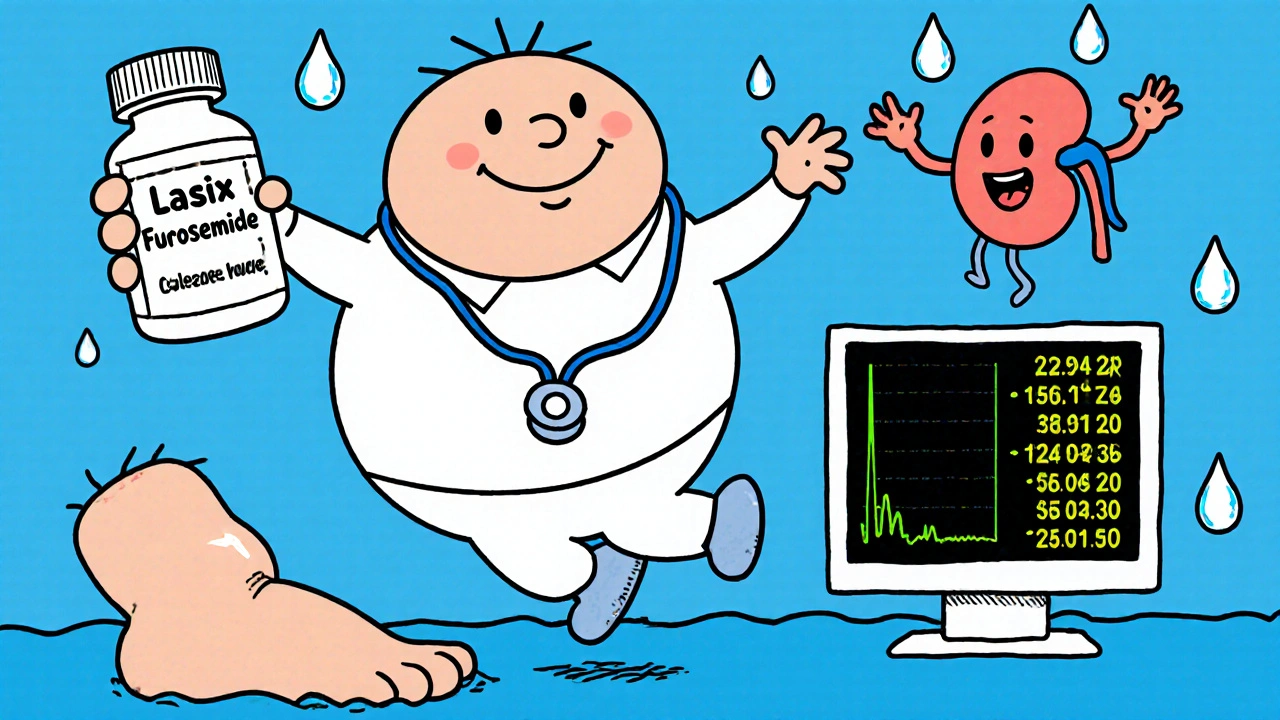
What Furosemide Actually Does
Furosemide, sold under brand names like Lasix, is a loop diuretic. That means it works in the loop of Henle in your kidneys - a key spot for filtering salt and water. It tells your kidneys to dump out more sodium and water than usual. This reduces swelling in your legs, eases pressure on your heart, and lowers blood pressure. It’s fast-acting: you’ll start peeing more within an hour, and the effect lasts 2-4 hours.
Doctors commonly prescribe it for:
- Heart failure
- Liver cirrhosis with fluid buildup
- Kidney disease
- High blood pressure (often combined with other drugs)
- Acute pulmonary edema (fluid in the lungs)
But it’s not perfect. Side effects like dizziness, low potassium, dehydration, and even hearing loss (rare but serious) are real risks. That’s why many patients and doctors look at alternatives.
Hydrochlorothiazide: The Mild Alternative
If you’re on a low dose of furosemide and just need a gentle nudge to get rid of extra fluid, hydrochlorothiazide (HCTZ) might be a better fit. It’s a thiazide diuretic - slower, gentler, and longer-lasting. It works in a different part of the kidney, so it doesn’t flush out as much potassium. That’s a plus.
But here’s the catch: HCTZ isn’t strong enough for severe swelling. If you’re in heart failure with major fluid overload, HCTZ won’t cut it. It’s better for mild hypertension or early-stage edema. Many doctors start with HCTZ for high blood pressure before moving to stronger drugs. It’s also cheaper and often available as a generic combo pill with ACE inhibitors or calcium channel blockers.
Side effects? Still possible: low sodium, high blood sugar, gout flare-ups. But overall, it’s less harsh on the body than furosemide.
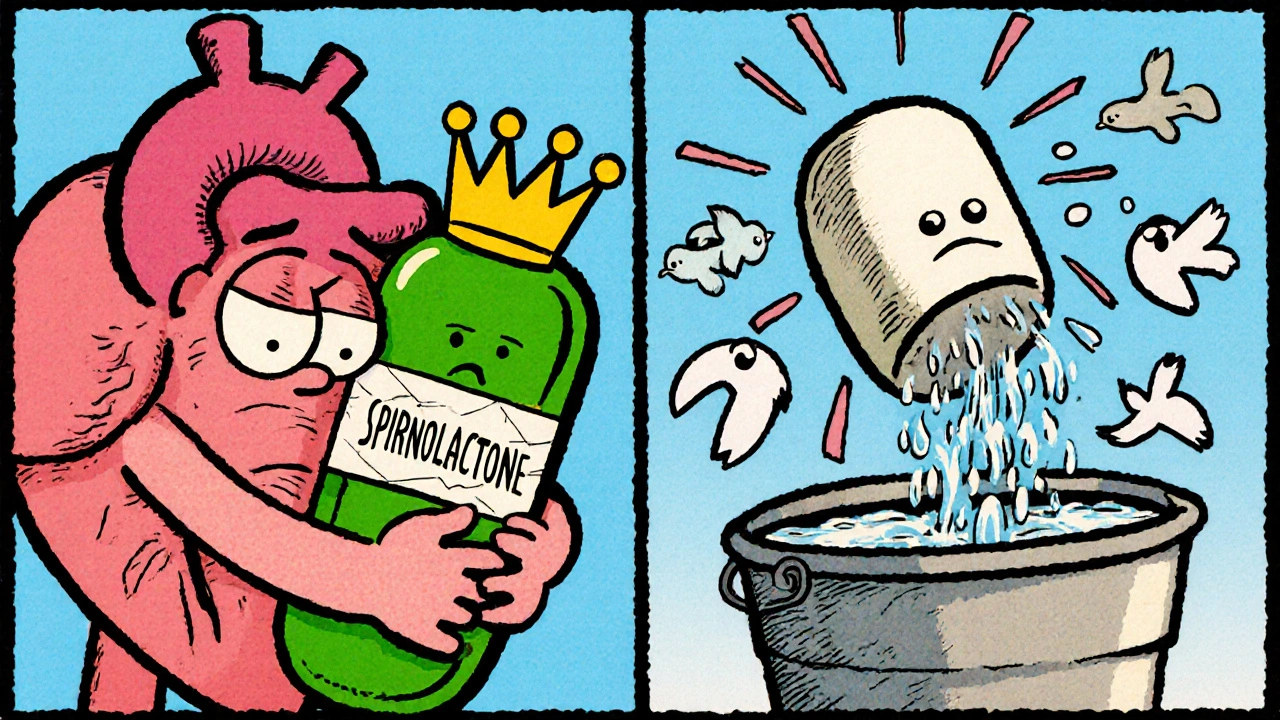
Spironolactone: The Potassium-Sparing Option
Spironolactone is not a typical diuretic. It’s an aldosterone blocker. Instead of forcing water out, it blocks a hormone that makes your body hold onto salt and water. This makes it slower to work - days, not hours - but it’s powerful for long-term fluid control, especially in heart failure.
It’s often used with furosemide. Why? Because furosemide drains potassium, and spironolactone saves it. Together, they balance each other. Studies like the RALES trial showed that adding spironolactone to standard heart failure treatment cut death risk by 30%. That’s huge.
But it has downsides. Men can get breast tenderness or enlargement. Women may have irregular periods. High potassium levels are a real concern, especially if you have kidney problems or take ACE inhibitors. You need regular blood tests. It’s not a first-line pick for everyone, but for certain heart patients, it’s life-changing.
Bumetanide: The Stronger Loop Diuretic
If furosemide isn’t doing enough, bumetanide might be the next step. It’s also a loop diuretic, but it’s about 40 times more potent. A 1 mg dose of bumetanide equals about 40 mg of furosemide. That means smaller pills, and sometimes fewer side effects from volume loss.
It’s often used in patients who’ve become resistant to furosemide - common in advanced heart failure or kidney disease. Bumetanide is also better absorbed when the gut is swollen (a problem in heart failure), so it works more reliably.
But it’s not a magic bullet. It still causes low potassium, dehydration, and dizziness. It’s also harder to get in some countries, and it’s more expensive. Not everyone’s doctor will try it first. But if you’ve hit a wall with furosemide, bumetanide is a solid next move.
Torsemide: The Long-Lasting Choice
Torsemide is another loop diuretic, but it has a longer duration - up to 8 hours. That means you might only need one dose a day, instead of two or three with furosemide. It’s also more completely absorbed from the gut, so it works more predictably.
Studies suggest torsemide may be better for heart failure patients long-term. One trial found fewer hospital readmissions with torsemide compared to furosemide. It also causes less potassium loss than furosemide. And unlike furosemide, it doesn’t seem to trigger as much of a stress response in the body’s hormone system.
It’s more expensive, but if you’re on daily diuretics and tired of timing doses around your schedule, torsemide simplifies things. Many patients report feeling more stable and less bloated throughout the day.
When to Stick With Furosemide
Just because alternatives exist doesn’t mean you should switch. Furosemide is still the most widely used, best-studied, and cheapest option. If it’s working for you - you’re not swollen, your blood pressure is under control, and you’re not having side effects - there’s no reason to change.
It’s also the standard in emergency settings. If someone shows up in the ER with sudden fluid overload, furosemide is the first drug they get. It’s fast, reliable, and available everywhere.
For many people, especially those on a fixed income, furosemide is the only practical option. Generic versions cost less than $5 a month in Australia. Alternatives like torsemide or bumetanide can cost 3-5 times more.
What Your Doctor Will Consider Before Switching
Switching diuretics isn’t just about what works best on paper. Your doctor looks at:
- How well you respond to furosemide now
- Your kidney function (eGFR)
- Your potassium and sodium levels
- Other meds you take (like ACE inhibitors or NSAIDs)
- Your lifestyle - can you handle multiple daily doses?
- Cost and access
If you’re on multiple diuretics, your doctor might try a combo. For example: furosemide in the morning, spironolactone at night. Or switch entirely to torsemide for simplicity.
Never switch on your own. Diuretics can cause dangerous electrolyte imbalances. Too little potassium can trigger irregular heartbeats. Too much can be just as risky. Monitoring is key.
Non-Drug Ways to Reduce Fluid Retention
Medications help, but they’re not the whole story. If you’re holding onto fluid, your diet matters.
- Salt intake: Less than 2,000 mg per day is ideal. Processed foods, canned soups, and takeaway meals are the biggest culprits.
- Fluid intake: Don’t overdrink unless you’re told to. For some with heart failure, limiting fluids to 1.5-2 liters a day helps.
- Weight tracking: Weigh yourself daily. A sudden 2 kg gain in 2 days means fluid is building up - call your doctor.
- Elevating legs: Helps with swelling in the ankles.
- Compression socks: Can reduce leg swelling without extra meds.
These aren’t replacements for diuretics, but they make them work better. Many patients find they need lower doses when they cut salt and monitor weight.
Final Thoughts: No One-Size-Fits-All
Furosemide isn’t outdated. But it’s not always the best. Alternatives like torsemide, bumetanide, and spironolactone have clear advantages in specific situations. Hydrochlorothiazide is great for mild cases. The right choice depends on your body, your health goals, and your daily life.
If you’re on furosemide and still feeling swollen, tired, or dizzy - talk to your doctor. Ask: "Is there a better option for me?" Don’t assume the first drug you got is the only one that works. With the right tweak, you might feel a lot better.
Can I switch from furosemide to hydrochlorothiazide on my own?
No. Switching diuretics without medical supervision can cause dangerous drops in blood pressure, dehydration, or electrolyte imbalances like low potassium or sodium. Always consult your doctor before changing your medication.
Which alternative to furosemide is safest for kidneys?
Torsemide and bumetanide are often preferred in kidney disease because they’re more reliably absorbed, even when the gut is swollen. Spironolactone can raise potassium levels, which can be risky if kidney function is poor. Your doctor will check your eGFR and potassium before choosing.
Is spironolactone better than furosemide for heart failure?
For many heart failure patients, yes - especially when used together. Spironolactone reduces long-term death risk by blocking harmful hormones, while furosemide quickly removes fluid. Studies show combining them improves survival more than furosemide alone.
Why does furosemide sometimes stop working?
This is called diuretic resistance. It happens when your body adapts - your kidneys start reabsorbing more salt, or swelling in your gut blocks absorption. Doctors may increase the dose, switch to a stronger diuretic like bumetanide, or add a second type like spironolactone.
Do any of the alternatives cause weight gain?
No - all diuretics help you lose fluid weight. But if you’re on spironolactone, you might notice slight breast tissue swelling in men, which can feel like weight gain. This isn’t fat - it’s fluid retention in tissue. It usually goes away if you stop the drug.

Michael Lynch
October 28, 2025 AT 08:03Been on furosemide for 3 years after my heart attack. Switched to torsemide last year and honestly? Life changed. No more 3x-a-day bathroom schedule, and my legs don’t feel like lead weights by afternoon. Worth the extra cost if your insurance covers it.
caroline howard
October 30, 2025 AT 07:48Oh sweetie, you’re telling me you didn’t know spironolactone can give men boobs? 😏 I mean, sure, it saves lives-but also your dignity. My uncle went from ‘I’m a tough guy’ to ‘I need a bra’ in six weeks. Worth it? Maybe. Comfortable? Nope.
Melissa Thompson
October 30, 2025 AT 17:50Anyone who thinks hydrochlorothiazide is a 'gentle' alternative clearly hasn't read the FDA black box warnings. HCTZ increases diabetes risk by 30% in elderly patients-especially those with metabolic syndrome. And don't get me started on how Americans treat diuretics like candy. This isn't a TikTok trend. It's pharmacology. Get educated.
Rika Nokashi
November 1, 2025 AT 15:28Let me tell you something, young people. In India, we used to treat fluid retention with coriander seeds and jeera water. No pills. No doctors. Just wisdom passed down for centuries. Now everyone wants the latest brand-name drug, and nobody remembers that salt is the real enemy. You think your kidneys are weak? Maybe it’s your masala chips. Cut the sodium. Drink water. Sleep with legs up. Simple. No pharmacy needed. Modern medicine has made us lazy.
Austin Levine
November 3, 2025 AT 14:59My dad’s on bumetanide now. Furosemide stopped working after his kidney decline. Bumetanide’s a beast-small pill, big effect. But he still checks his potassium daily. No shortcuts.
Matthew King
November 4, 2025 AT 10:00bro i just take my lasix and chill. why complicate it? if it aint broke dont fix it. also i drink 3 liters of water a day because my nurse said so. idk if that’s right but i’m not dying so 🤷♂️
Gurupriya Dutta
November 5, 2025 AT 14:25I’ve been on spironolactone for a year now. At first, I was scared of the side effects-especially since I’m a woman. But my doctor explained it’s not just about fluid-it’s about hormones. I feel more balanced overall. Not just less swollen, but less anxious, less bloated emotionally too. It’s not magic, but it’s been a quiet game-changer.
Jenn Clark
November 5, 2025 AT 17:26My grandmother in Nigeria used to make a tea from hibiscus flowers for swelling. She said it was like nature’s diuretic. I didn’t believe her until I started drinking it daily-alongside my meds. My legs didn’t swell as bad. Not a replacement, but a gentle helper. Maybe we’ve forgotten how to use food as medicine.
Meredith Poley
November 7, 2025 AT 07:16Oh wow, someone actually mentioned non-drug methods? Shocking. Most people think popping a pill is the only way. Cut the salt. Weigh daily. Elevate your legs. These aren’t ‘alternative therapies’-they’re the foundation. If you’re not doing these, no diuretic will save you. Just saying.
Amelia Wigton
November 8, 2025 AT 00:23According to the 2023 ACC/AHA Heart Failure Guidelines, Section 4.2.7, loop diuretics remain first-line for acute decompensated HF, but in chronic HFrEF, the class I recommendation for MRAs (e.g., spironolactone) is now Grade A, Level 1 evidence. Torsemide’s pharmacokinetic superiority over furosemide is documented in the TORCH trial (2021 meta-analysis) with a 22% reduction in HF hospitalizations. You cannot make clinical decisions without referencing the evidence base.
L Walker
November 8, 2025 AT 07:29My GP switched me from furosemide to torsemide after I kept getting cramps. One pill a day. No more midnight bathroom runs. I didn’t even know it was an option. Why isn’t this talked about more?
Andrea Swick
November 9, 2025 AT 12:12It’s funny how people act like furosemide is the villain. It’s been saving lives for 70 years. The problem isn’t the drug-it’s that we treat symptoms without fixing root causes. Why are we so quick to swap pills instead of asking why the body’s holding fluid in the first place? Maybe it’s the sugar. Maybe it’s the stress. Maybe it’s the fact we sit all day. We’re so focused on the ‘how’ we forget the ‘why’.
Mathias Matengu Mabuta
November 10, 2025 AT 20:51Let me be clear: this entire post is dangerously oversimplified. Furosemide is not 'cheap' in most of the world-especially in countries without universal healthcare. Torsemide’s cost-effectiveness is only valid in the U.S. insurance system. In India, spironolactone is often unavailable due to supply chain issues. And the notion that 'non-drug methods' are sufficient? That’s a privilege of the healthy and the insured. Don’t preach to people who can’t afford to cut salt because their only food option is instant noodles.
james landon
November 12, 2025 AT 19:05so like… if i just drink less water, will i stop swelling? 😅
Don Moore
November 13, 2025 AT 09:52Thank you for this thorough breakdown. As a healthcare provider, I appreciate when patients come in with informed questions. The key takeaway remains: individualization is everything. What works for one body may harm another. Always consult your provider before adjusting therapy. Diuretics are powerful tools-but they demand respect.