Trying to get pregnant? If you’ve been trying for months without success, it’s easy to blame stress, timing, or bad luck. But there’s one hidden factor many doctors overlook: your thyroid. Specifically, your TSH level. For women planning pregnancy, TSH isn’t just a number on a lab report-it’s a silent gatekeeper to fertility and a healthy pregnancy.
Why TSH Matters More Than You Think
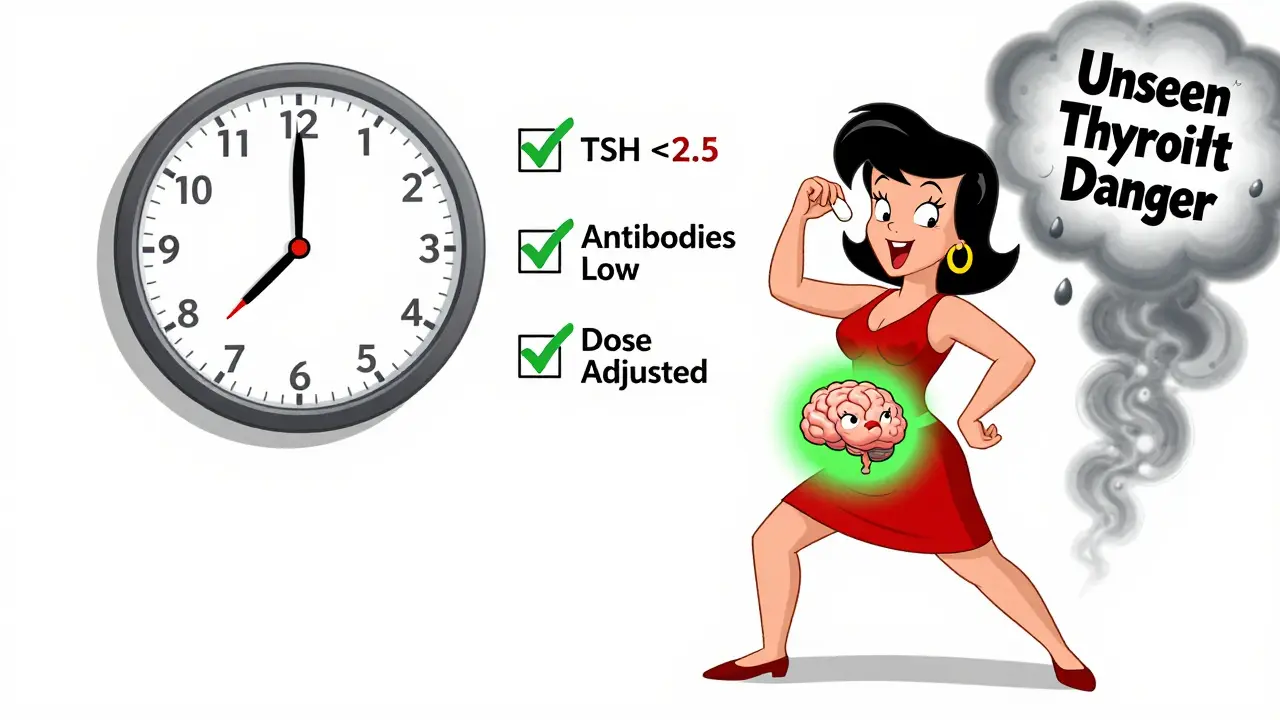
TSH, or thyroid-stimulating hormone, is the signal your brain sends to your thyroid to make hormones. When TSH is too high, your thyroid isn’t working hard enough. That’s hypothyroidism. Even if your TSH is in the "normal" range-say, 3.0 or 3.5-it might still be too high for conception. The American Thyroid Association (ATA) says women trying to get pregnant should aim for a TSH level under 2.5 mIU/L. That’s not the same as the general population range (usually 0.4-4.5 mIU/L). Why the difference? Because your body needs more thyroid hormone during early pregnancy. Your baby can’t make its own thyroid hormones until about 12 weeks. Until then, it’s completely dependent on you. A 2018 study of over 7,000 women found that those with unexplained infertility were nearly twice as likely to have TSH levels above 2.5 mIU/L compared to women who conceived easily. That’s not coincidence. Low thyroid hormone slows down ovulation, messes with egg quality, and can throw off your menstrual cycle. The Mayo Clinic puts it simply: "Low thyroid hormone can interfere with the release of an egg from your ovary."What If You Have Hashimoto’s?
If you have Hashimoto’s thyroiditis-an autoimmune condition where your immune system attacks your thyroid-you’re at even higher risk. Studies show that women with Hashimoto’s need even tighter control before pregnancy. Experts recommend keeping TSH between 1.25 and 1.75 mIU/L, not just under 2.5. Why? Because your thyroid is already damaged. During pregnancy, your body’s demand for thyroid hormone jumps by 30-50%. If you’re already running low, you’ll crash faster. One 2023 study from the American Thyroid Association found that women with Hashimoto’s who didn’t optimize their TSH before conception were far more likely to miscarry or deliver prematurely. And it’s not just about TSH. Your thyroid antibodies (TPOAb) matter too. Even if your TSH is normal, high antibodies can increase your risk of miscarriage by up to 50%. That’s why testing for both TSH and antibodies is critical if you have a history of autoimmune disease.The Levothyroxine Trap
If you’re already on levothyroxine (the standard thyroid hormone replacement), you might think you’re covered. But here’s the catch: most women need a 25-50% dose increase as soon as they get pregnant. Yet, a 2019 study found that only 37% of women got their dose adjusted in time. Many waited until their first prenatal visit-by then, it might be too late. Why does this happen? Doctors often don’t realize how quickly thyroid needs change. Your body starts producing more thyroid-binding proteins as soon as you conceive. That means more hormone gets bound up and becomes inactive. Your thyroid has to work harder, and if it’s already compromised, you’ll need more medication. The fix? Don’t wait. If you’re planning pregnancy, talk to your doctor now. Get your TSH checked, and if you’re on levothyroxine, ask if your dose needs adjusting. Once you’re pregnant, retest every 4 weeks until you hit 20 weeks. Most women need a dose increase within the first 6 weeks. And don’t use desiccated thyroid (like Armour Thyroid). It’s not stable enough for pregnancy. The InVia Fertility Center and other top reproductive clinics specifically warn against it because it lowers serum T4-the hormone your baby needs most.
Screening: Should Everyone Get Tested?
The American College of Obstetricians and Gynecologists (ACOG) doesn’t recommend universal TSH screening for all women trying to conceive. But the American Society for Reproductive Medicine (ASRM) does. And here’s why the debate matters: about 15-20% of women with infertility have abnormal TSH levels. That’s one in five. And thyroid dysfunction is one of the few fertility issues you can fix with a simple, cheap pill. If you have any of these risk factors, get tested:- History of thyroid disease or family history of it
- Unexplained infertility
- Irregular periods or very light bleeding
- Unexplained fatigue, weight gain, or hair loss
- Previous miscarriage
- Autoimmune conditions like type 1 diabetes or celiac disease
What About TSH Between 2.5 and 4.5?
This is where things get messy. Some studies say it’s fine. Others say it’s risky. A 2017 study of women undergoing IUI found no difference in pregnancy or live birth rates between those with TSH under 2.5 and those between 2.5 and 4.5. That study got a lot of attention. But it had a small sample size and didn’t look at miscarriage rates. Meanwhile, a massive 2018 study of over 180,000 women found that those with TSH between 2.5 and 4.5 had a 15% higher risk of miscarriage. That’s not trivial. And if you have thyroid antibodies? The risk jumps even higher. Here’s the bottom line: if your TSH is 3.0 or above and you’re trying to conceive, don’t wait for symptoms. Ask your doctor to treat it. Levothyroxine is safe, cheap, and effective. A 2021 meta-analysis showed that treating subclinical hypothyroidism in infertile women reduced miscarriage rates by 45% and improved live birth rates by 36%.How to Get Your TSH Right
If you’re planning pregnancy, here’s your step-by-step plan:- Get your TSH and TPOAb tested. Don’t skip the antibodies.
- If your TSH is above 2.5, talk to your doctor about starting or adjusting levothyroxine.
- If you have Hashimoto’s, aim for 1.25-1.75 mIU/L.
- Take levothyroxine on an empty stomach with water. Wait at least 30 minutes before eating or taking other meds.
- Avoid calcium, iron, or antacids within 4 hours of your dose-they block absorption.
- Retest every 4 weeks until your TSH is stable under 2.5.
- Once pregnant, retest every 4 weeks until week 20. Dose will likely need increasing.



Isaac Jules
January 6, 2026 AT 09:42This is the kind of bullshit that makes me want to scream. TSH under 2.5? Who the fuck decided that? My doctor said 4.0 is fine and I’ve been trying for 18 months. Now I’m supposed to believe some random study from 2018 is gospel? 😤
Amy Le
January 7, 2026 AT 09:05Wow. Just… wow. 🤯 So let me get this straight - we’re supposed to treat a hormone like it’s a dial on a radio, turning it down to ‘baby mode’? This isn’t medicine, it’s bio-optimization cultism. And why are we ignoring the fact that TSH fluctuates naturally? 😒
Pavan Vora
January 9, 2026 AT 02:02Interesting… very interesting… 😊 I come from India, where many women just… try, and get pregnant, without any testing… TSH? What is that? We have chai, prayers, and patience… 🙏 Maybe… maybe… too much science is not always better? 🤔
Stuart Shield
January 10, 2026 AT 06:13Man, this is the kind of post that makes you feel like you’ve been walking through a fog your whole life. Thyroid health? I never connected my exhaustion, hair loss, and mood swings to this. I thought I was just ‘burnt out.’ Turns out, my body was screaming and I was too busy scrolling to hear it. Thanks for the clarity.
Indra Triawan
January 10, 2026 AT 10:39Oh my god, I’ve been doing everything right - diet, yoga, supplements, timing… and now I find out my TSH was 3.2 the whole time? Like… I’m not even mad. I’m just… hollow. 😔
Susan Arlene
January 11, 2026 AT 09:52so i got my tsh tested last month and it was 3.1… doc said ‘eh, fine’… i just… i don’t know anymore. i’m tired. 🥱
Joann Absi
January 12, 2026 AT 00:21THEY’RE HIDING THIS FROM US!! 🚨 WHY ISN’T THIS ON EVERY WOMAN’S OB-GYN CHECKLIST?! WHY DO WE HAVE TO FIND THIS ON REDDIT?! THIS IS A NATIONAL SCANDAL!! I’M STARTING A PETITION!! 🗣️💥
Mukesh Pareek
January 12, 2026 AT 10:12It’s a classic case of subclinical hypothyroidism with a potential autoimmune component, as evidenced by the elevated TPOAb titers. The TSH threshold of 2.5 mIU/L is not arbitrary - it’s derived from a meta-analysis of eutrophic reproductive cohorts with controlled confounders. Failure to intervene constitutes a violation of the precautionary principle in reproductive endocrinology.
Rachel Wermager
January 13, 2026 AT 07:44Actually, the 2.5 cutoff is outdated. The 2022 ATA guidelines now recommend 2.0 for conception, and 1.5 for those with TPOAb+. You’re not optimizing - you’re just following the minimum. And if your doctor doesn’t know that, they’re not qualified to manage your care.
Katelyn Slack
January 14, 2026 AT 11:20thank you for this… i had no idea… i’m going to ask my doctor for the tpoab test tomorrow… i’ve had so many miscarriages… i just thought it was bad luck…
Melanie Clark
January 15, 2026 AT 14:30This is all part of the pharmaceutical-industrial complex. Levothyroxine is a billion-dollar drug. They’re pushing this to sell pills. Did you know the FDA changed the reference ranges because of lobbying? Wake up. Your body knows what it needs. You don’t need a pill to get pregnant. You need to detox, eat clean, and trust your intuition.
Harshit Kansal
January 17, 2026 AT 14:26bro i just tried this last year and got pregnant in 2 months. no meds. just chill vibes and good sleep. maybe you’re stressing too hard? try yoga. or just go on vacation. life is short.
Brian Anaz
January 19, 2026 AT 06:54So if you’re over 2.5, you’re broken? That’s the message here? What about women who live in places without labs or doctors? Are they just not allowed to have kids? This feels like rich white woman medicine.
Vinayak Naik
January 20, 2026 AT 22:03Man, I’m a nurse in Delhi and I’ve seen this a hundred times - women come in with TSH at 4.0, hair falling out, skin like paper, and the doc says ‘you’re fine.’ Then they cry for 2 years. I wish I could hand every woman a blood test form and say ‘do this, please.’
Saylor Frye
January 21, 2026 AT 15:00Look, I get it. But this feels like another wellness influencer pushing a ‘biohacked fertility’ narrative. Next they’ll be telling us to align our menstrual cycles with the moon and drink celery juice before ovulation. It’s not magic. It’s science. And science says: if you’re asymptomatic and your TSH is under 4.5, you’re fine.