If you’re taking a DPP-4 inhibitor for type 2 diabetes, you might not realize that joint pain could be linked to your medication. It’s not a common side effect, but when it happens, it can be severe enough to stop you from walking, working, or even getting out of bed. The FDA first flagged this risk in 2015, and since then, doctors and patients have learned to watch for it - not just in the first few weeks, but even after months or years of use.
What Are DPP-4 Inhibitors?
DPP-4 inhibitors are oral diabetes drugs that help control blood sugar by boosting natural hormones that tell your body to release insulin after meals. They don’t cause weight gain or low blood sugar on their own, which is why many doctors still prescribe them. Common brands include Januvia (sitagliptin), Onglyza (saxagliptin), Tradjenta (linagliptin), and Nesina (alogliptin). Vildagliptin (Galvus) is used outside the U.S. but works the same way.
These drugs are popular because they’re well-tolerated. Most people report mild side effects like a stuffy nose, headache, or upset stomach. But for a small number, something more serious shows up: intense, unexplained joint pain.
The FDA Warning: What Changed in 2015
In August 2015, the U.S. Food and Drug Administration (FDA) issued a safety alert after reviewing over 7 years of reports. They found 33 cases of severe joint pain directly tied to DPP-4 inhibitors. That might sound like a tiny number - but here’s what made it alarming:
- 28 cases involved sitagliptin (Januvia)
- 5 involved saxagliptin (Onglyza)
- 2 involved linagliptin (Tradjenta)
- 1 involved alogliptin (Nesina)
- 2 involved vildagliptin
Five patients had the pain return after restarting the same drug - a classic sign of a drug-caused reaction. In 23 of the 33 cases, pain went away within a month of stopping the medication. Ten patients needed hospital care. One woman developed severe knee pain three weeks after starting Januvia. When she stopped it, the pain vanished. When she accidentally took it again, the pain came back in 48 hours.
The FDA didn’t pull these drugs off the market. Instead, they updated the labels to warn doctors and patients: severe joint pain is a real possibility.
How Bad Is the Joint Pain?
This isn’t the kind of ache you get after a long walk. Patients describe it as:
- Deep, constant, and burning
- Affecting multiple joints - knees, hips, hands, shoulders
- Worse at night or with movement
- So intense it stops daily activities
Some people were misdiagnosed with rheumatoid arthritis, lupus, or gout. One patient spent months seeing specialists, getting MRIs, and taking anti-inflammatory drugs - until her doctor asked if she’d started any new medications. That’s when the link clicked.
Unlike arthritis, this pain doesn’t usually cause swelling or redness. That’s why it’s easy to miss. It’s not an immune attack on the joints - it’s a reaction triggered by the drug.
When Does the Pain Start?
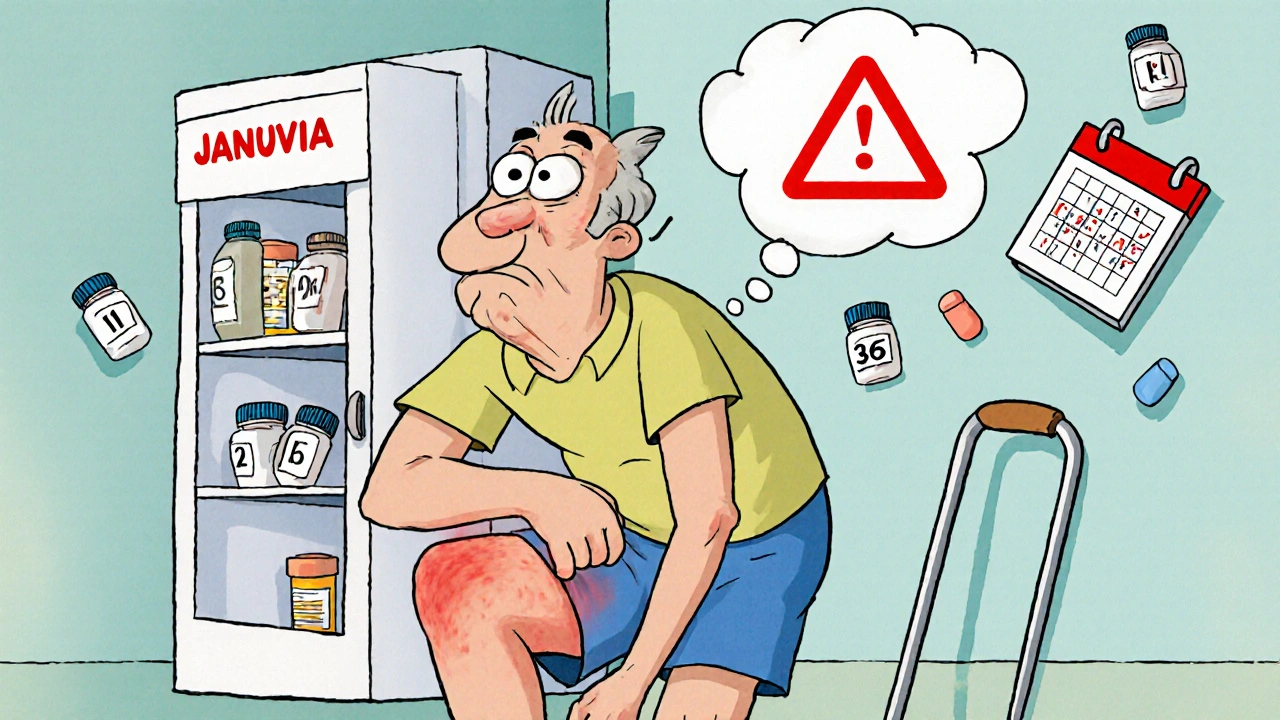
Most people think side effects show up right away. But with DPP-4 inhibitors, joint pain can appear anytime:
- Within the first month (22 out of 33 cases)
- After 6 months or even a year
This delay is one reason why it’s often overlooked. If you’ve been on Januvia for a year and suddenly can’t climb stairs, you might blame aging, overuse, or arthritis. But if you’ve had no prior joint issues, it’s worth asking: Could this be the drug?
What Do Studies Say?
Some studies back up the FDA’s warning. A 2021 analysis using data from over 250 million Americans found that people taking DPP-4 inhibitors had a 24% higher risk of needing medical care for joint pain compared to those on other diabetes drugs.
But not all research agrees. A large study in Taiwan found no clear link, possibly because doctors misclassified joint pain in medical records. Another study showed a small increase in joint discomfort (13% higher risk), but not the severe, disabling kind.
Here’s the key: the FDA’s data came from real-world reports - not clinical trials. That means they saw what actually happened to people using these drugs in daily life, not under controlled conditions. And the pattern was clear: stop the drug, pain fades. Restart it, pain returns.
What Should You Do If You Have Joint Pain?
Don’t stop your medication on your own. But do contact your doctor right away if you notice:
- New, unexplained joint pain
- Pain that’s worse than normal aging or injury
- Pain that doesn’t improve with rest or over-the-counter painkillers
Your doctor may ask you to stop the DPP-4 inhibitor for a few weeks to see if the pain improves. If it does, they’ll likely switch you to another diabetes drug - like an SGLT2 inhibitor (e.g., Jardiance) or a GLP-1 receptor agonist (e.g., Ozempic). These alternatives don’t carry the same joint pain risk.
If you’ve had this reaction before, avoid all DPP-4 inhibitors. The risk isn’t just with one brand - it’s class-wide.

Other Side Effects to Watch For
While joint pain is the most serious and under-recognized side effect, DPP-4 inhibitors can also cause:
- Pancreatitis (inflammation of the pancreas)
- Severe allergic reactions (swelling, trouble breathing)
- Bullous pemphigoid (a skin condition with blisters and sores)
- Low blood sugar (if taken with sulfonylureas like glipizide)
If you develop blisters, skin peeling, or sudden swelling, seek medical help immediately. These are rare but dangerous.
Is It Still Safe to Take DPP-4 Inhibitors?
Yes - for most people. The FDA still says the benefits outweigh the risks. Over 35 million prescriptions for sitagliptin are filled each year in the U.S. alone. That means millions are using these drugs safely.
The risk of severe joint pain is low - estimated at less than 1 in 1,000 users. But if you’re one of them, it’s life-changing. That’s why awareness matters.
If you’ve been on a DPP-4 inhibitor for a while and feel fine, keep taking it. But if you’ve had unexplained joint pain, even once, talk to your doctor. Don’t assume it’s just aging. Don’t wait until it’s crippling.
What’s Next?
Researchers are now working on better ways to identify who’s at risk. The American College of Rheumatology is developing diagnostic criteria to help doctors tell DPP-4 inhibitor pain apart from arthritis. Real-time monitoring systems like the FDA’s Sentinel Initiative are tracking more cases as they happen.
For now, the best protection is knowledge. If you’re on one of these drugs, pay attention to your body. If something feels off - especially in your joints - speak up. It could save you months of pain and unnecessary tests.
Can DPP-4 inhibitors cause joint pain even after years of use?
Yes. While many cases start within the first month, the FDA has documented joint pain appearing after 6 months or even a year of use. This delay makes it harder to connect the symptom to the drug, so it’s important to consider DPP-4 inhibitors as a possible cause no matter how long you’ve been taking them.
Should I stop taking my DPP-4 inhibitor if I have joint pain?
No - don’t stop on your own. Contact your doctor right away. They may recommend stopping the drug temporarily to see if your pain improves. If it does, they’ll switch you to a safer alternative. Stopping without medical guidance can cause your blood sugar to spike.
Is joint pain from DPP-4 inhibitors permanent?
In most cases, no. Of the 33 severe cases reviewed by the FDA, 23 resolved within a month of stopping the drug. Only 8 patients had pain return after restarting the medication. For most people, the pain fades completely once the drug is out of their system.
Are all DPP-4 inhibitors equally likely to cause joint pain?
The FDA found that the risk appears to be class-wide. While sitagliptin had the most reports, cases were also linked to saxagliptin, linagliptin, alogliptin, and vildagliptin. If you’ve had joint pain with one DPP-4 inhibitor, you should avoid all of them.
What are safer alternatives to DPP-4 inhibitors?
Alternatives include SGLT2 inhibitors like Jardiance or Farxiga, GLP-1 receptor agonists like Ozempic or Trulicity, metformin, or insulin. These don’t carry the same joint pain risk and can be just as effective. Your doctor can help choose the best option based on your health, cost, and other conditions.
How common is joint pain with DPP-4 inhibitors?
Mild joint discomfort occurs in about 5-10% of users, but severe, disabling pain is rare - likely less than 1 in 1,000. Still, because over 35 million prescriptions are filled each year in the U.S., even a small percentage means thousands of people could be affected. Awareness is key to catching it early.

Johnson Abraham
November 14, 2025 AT 06:13Shante Ajadeen
November 16, 2025 AT 02:55dace yates
November 16, 2025 AT 18:23Danae Miley
November 16, 2025 AT 19:33Charles Lewis
November 17, 2025 AT 01:07Renee Ruth
November 17, 2025 AT 13:55Samantha Wade
November 17, 2025 AT 17:57Elizabeth Buján
November 17, 2025 AT 21:05Andrew Forthmuller
November 19, 2025 AT 11:56vanessa k
November 20, 2025 AT 01:42manish kumar
November 21, 2025 AT 06:56Nicole M
November 22, 2025 AT 02:42Arpita Shukla
November 23, 2025 AT 19:21Benjamin Stöffler
November 24, 2025 AT 02:08