Managing diabetes doesn’t mean giving up your favorite foods. It means learning how to work with them. One of the most effective, flexible, and widely recommended tools for doing this is carbohydrate counting. If you’re new to diabetes management, you might feel overwhelmed by numbers, labels, and meal plans. But carb counting isn’t about perfection-it’s about understanding how food affects your blood sugar so you can make smarter choices, day after day.
What Is Carbohydrate Counting?
Carbohydrate counting, or carb counting, is a simple idea with powerful results: you track how many grams of carbs you eat at each meal and snack, then match that to your insulin or other diabetes medication. Carbs are the main nutrient that raises blood sugar after eating. Whether it’s bread, rice, fruit, or yogurt, they all break down into glucose-and that glucose enters your bloodstream quickly.
One standard serving of carbs equals about 15 grams. That’s:
- 1 slice of bread
- 1 small apple
- 1/2 cup of cooked rice or pasta
- 1/2 cup of beans
- 1 cup of milk
You don’t need to count every single bite right away. Start by learning what 15 grams looks like on your plate. Over time, you’ll get better at estimating. The goal isn’t to become a human nutrition label-it’s to gain control over your blood sugar without feeling restricted.
Why It Works for Diabetes
When you eat carbs, your blood sugar rises. If you take insulin, your body needs a certain amount to handle that rise. Too little insulin? Blood sugar spikes. Too much? You risk low blood sugar. Carb counting gives you the exact numbers you need to match your insulin dose to your food.
People with type 1 diabetes rely on this method because their bodies don’t make insulin at all. Many with type 2 diabetes who use insulin also benefit. Even if you’re not on insulin, knowing your carb intake helps you understand why your blood sugar goes up after certain meals.
Research shows that people who track their carbs consistently see better results. Studies from the American Diabetes Association found that carb counting can lower HbA1c (a 3-month blood sugar average) by 0.5% to 1.0%. That might sound small, but it cuts your risk of complications like nerve damage, kidney problems, and vision loss.
How to Read Nutrition Labels for Carb Counting
You don’t need to guess. Food labels tell you exactly what you need.
Look for the line that says “Total Carbohydrate”. That number includes all carbs: sugars, starches, and fiber. You don’t need to add them up yourself-the label does it for you.
Here’s where it gets practical:
- If a food has 5 grams or more of fiber per serving, subtract the full fiber amount from the total carbs. Fiber doesn’t raise blood sugar.
- If it contains sugar alcohols (like erythritol or maltitol), subtract half of that amount. They have less impact on blood sugar than regular sugar.
Example: A yogurt has 20g total carbs, 4g fiber, and 6g sugar alcohols.
Net carbs = 20 - 4 - (6 ÷ 2) = 20 - 4 - 3 = 13g net carbs.
That’s your real carb count for insulin dosing or tracking.
Your Carb-to-Insulin Ratio: The Key to Precision
If you take insulin, your doctor or diabetes educator will give you a carb-to-insulin ratio. This tells you how much insulin you need per gram of carbs.
For example:
- A ratio of 1:10 means 1 unit of insulin covers 10 grams of carbs.
- A ratio of 1:15 means 1 unit covers 15 grams.
If you eat 45 grams of carbs and your ratio is 1:15, you take 3 units of insulin (45 ÷ 15 = 3).
This ratio isn’t the same for everyone. It can change based on:
- Time of day (many people need more insulin at dinner than breakfast)
- Activity level
- Insulin type and how your body responds
Your care team will help you find your starting ratio, then adjust it over time based on your blood sugar logs.

Tools You Need to Get Started
You don’t need fancy gear. But having the right tools makes accuracy easier.
- A food scale (for weighing meats, cheese, and cooked grains)
- Measuring cups and spoons (for rice, pasta, cereal, fruit)
- A calculator (or your phone’s calculator app)
- A food diary or app (to log meals and blood sugar)
Apps like MyFitnessPal, Carb Manager, or the USDA’s FoodData Central are free and packed with data. Carb Manager’s SmartScan feature even lets you take a photo of your meal and gets an estimated carb count using AI-about 85% accurate, according to independent testing.
Start by measuring everything for 1-2 weeks. You’ll be surprised how much you over- or underestimate. A small bowl of oatmeal might be 2 servings. A restaurant side of mashed potatoes could be 3 servings. Once you’ve measured, you’ll start to recognize portions by sight.
Common Mistakes and How to Avoid Them
Most beginners make the same errors. Here’s how to dodge them:
- Forgetting hidden carbs: Milk in coffee, yogurt, sauces, starchy veggies (like corn or peas), and even some medications contain carbs. These add up fast.
- Not counting all meals: Skipping snacks or “just a bite” can throw off your numbers. Every carb counts.
- Trusting restaurant labels: Chain restaurants often list carb counts that are too low. A “small” burger bun might be 30g carbs, not 15. Always assume it’s higher than stated.
- Ignoring fiber and sugar alcohols: If you don’t subtract them, you’ll take too much insulin and risk low blood sugar.
Keep a log of what you eat, your insulin dose, and your blood sugar 2 hours after eating. Look for patterns. If your blood sugar is high after pasta but fine after quinoa, you’re learning how different carbs affect you.
Carb Counting vs. Other Methods
There are other ways to manage food with diabetes:
- The Plate Method: Fill half your plate with non-starchy veggies, a quarter with protein, a quarter with carbs. Simple, but doesn’t give you exact numbers for insulin.
- Glycemic Index (GI): Focuses on how fast carbs raise blood sugar. But two foods with the same GI can have totally different carb amounts. GI doesn’t help you dose insulin.
Carb counting wins because it’s precise and flexible. You can eat pizza, pasta, or cake-as long as you know how many carbs are in it and adjust your insulin. That’s the freedom it gives you.
What to Expect in the First 30 Days
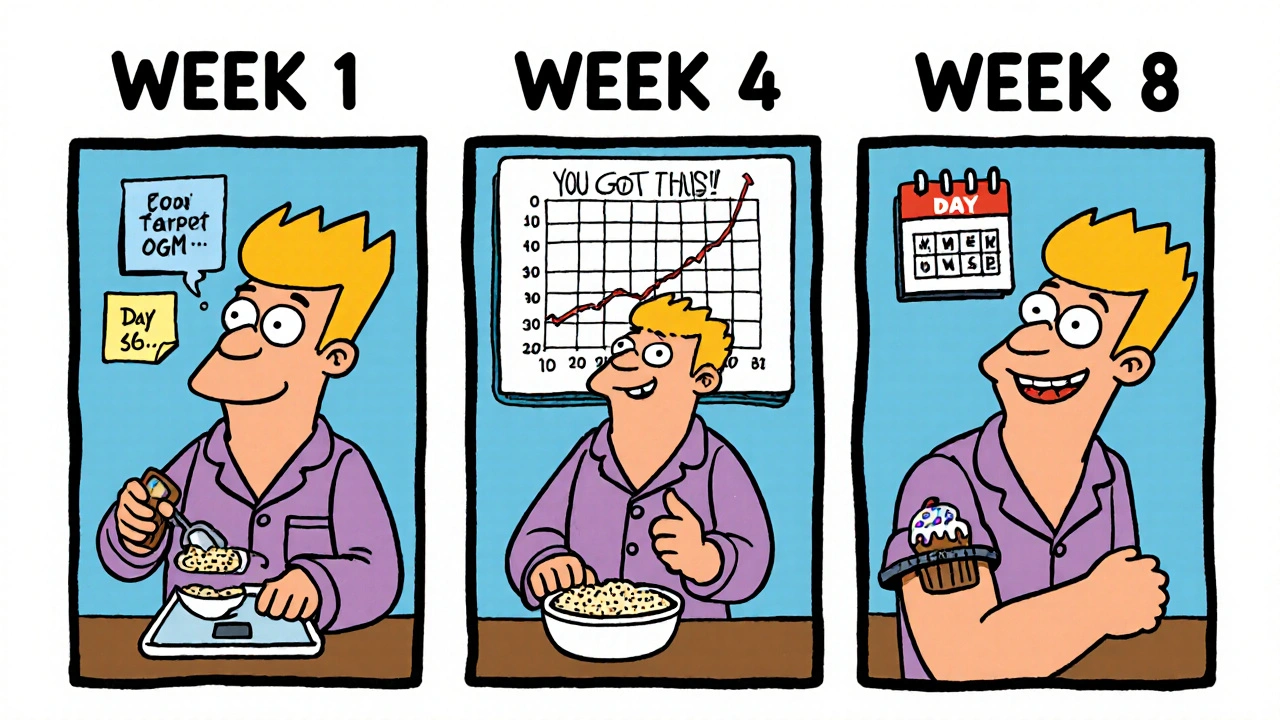
You won’t master this overnight. Most people take 4-8 weeks to feel confident. Here’s what to expect:
- Week 1-2: You’ll measure everything. Meals take 30-60 minutes. You’ll feel tired of counting.
- Week 3-4: You’ll start recognizing portions. You’ll notice which foods spike your blood sugar more than others.
- Week 5-8: You’ll estimate accurately 80-85% of the time. You’ll feel in control.
One person on Reddit shared: “My post-meal spikes dropped from 250+ to 160-180 in two weeks. I didn’t change my food-I just started counting.”
That’s the power of knowing your numbers.
When Carb Counting Might Not Be Right for You
It’s not for everyone. If you have type 2 diabetes and manage it with diet and oral meds (like metformin), you might not need to count every gram. The plate method or simple portion control may be enough.
But if you’re on insulin-especially multiple daily injections or an insulin pump-carb counting is the gold standard. It’s taught in 92% of ADA-recognized diabetes education programs. And with continuous glucose monitors (CGMs) now common, you can see real-time feedback: Did your carb count match your insulin? Did your blood sugar stay steady?
Carb counting isn’t just a diet plan. It’s a skill. And like any skill, it gets easier with practice.
Next Steps: Start Today
Here’s your simple 3-step plan to begin:
- Get your carb-to-insulin ratio from your doctor or diabetes educator. If you don’t have one, ask for it.
- Buy a food scale and measuring cups. Use them for 10 days. Measure everything.
- Download a free carb-tracking app and log your meals and blood sugar. Review your log weekly with your care team.
You don’t need to be perfect. You just need to be consistent. The goal isn’t to eliminate carbs-it’s to understand them. And when you do, you’re no longer at the mercy of your blood sugar. You’re in charge.
Do I need to count carbs if I’m not on insulin?
Not necessarily. If you manage type 2 diabetes with diet, exercise, or oral medications like metformin, you may not need precise carb counting. Instead, focus on portion control, choosing whole grains and vegetables, and avoiding sugary drinks. But even without insulin, tracking carbs can help you see which foods cause spikes-and make smarter choices.
Can I still eat sweets and desserts with carb counting?
Yes. Carb counting gives you the freedom to enjoy treats-you just need to account for the carbs. A small slice of cake might be 30 grams of carbs. If your ratio is 1:10, you’d take 3 units of insulin for it. Many people use this method to have pizza night, birthday cake, or ice cream without guilt. The key is matching insulin to the carb amount, not avoiding the food entirely.
How do I count carbs in restaurant meals?
Most chain restaurants list nutrition info online-check their website before you go. For non-chain places, estimate based on what you know: a serving of rice is about 45g carbs, a bun is 30g, and a side of fries is 40-50g. When in doubt, assume it’s more than labeled. Use a food scale at home to learn what portions look like, so you can guess better out. Always log what you eat and check your blood sugar afterward to learn from each experience.
What if I forget to count carbs before eating?
If you’ve already eaten and didn’t count, don’t panic. Check your blood sugar 2 hours later. If it’s high, you can take a correction dose of insulin (if your care team has given you a correction factor). Then, write down what you ate and how much. Use that info to plan better next time. It’s not about being perfect-it’s about learning from every meal.
How long does it take to get good at carb counting?
Most people reach 80-85% accuracy after 30 days of consistent practice. The first week is the hardest-you’ll measure everything. By week four, you’ll start recognizing portions by sight. After two months, you’ll be estimating meals quickly and confidently. It’s a skill that becomes second nature.



Sam Jepsen
November 24, 2025 AT 06:21Man I wish I had this guide when I was first diagnosed. I used to just guess and end up crashing or spiking like a rocket. Now I use Carb Manager and it’s a game changer. Started with measuring everything and now I can eyeball a plate and be within 5g. No more fear of pizza night 😎
Yvonne Franklin
November 25, 2025 AT 19:42Net carbs matter more than total. Always subtract fiber and half the sugar alcohols. That one trick saved me from 3 hypoglycemic episodes last month
Shawn Daughhetee
November 26, 2025 AT 13:04I used to think carb counting was for people who wanted to be perfect. Turns out it’s just about being less surprised by your numbers. My A1c dropped from 8.2 to 6.9 in 3 months just by knowing what I was eating. No magic, just math
Justin Daniel
November 28, 2025 AT 00:13They say carb counting gives you freedom but honestly it feels like a full time job at first. I used to hate logging meals. Now I do it while scrolling TikTok. Funny how your brain adapts. Also yes you can eat cake. I had a slice last night. Took 2 units. Blood sugar was 152 two hours later. Victory
Melvina Zelee
November 28, 2025 AT 16:36so like i was just reading this and it hit me-i dont need to be perfect, i just need to be aware. i used to eat pasta and then wonder why i felt like a zombie. now i know its not the pasta, its the portion. and the fact i forgot the fiber in the sauce. lol. also i started using my phone to scan barcodes and its like having a nutritionist in my pocket. 10/10 would recommend. dont stress just start small
ann smith
November 29, 2025 AT 10:28This is such a thoughtful, clear guide. I’m so glad you shared this. For anyone feeling overwhelmed-just pick one thing to start with. Maybe just measure your rice for a week. Small steps lead to big changes. You’ve got this 💪
Julie Pulvino
November 30, 2025 AT 11:23I’m type 2 and on metformin. I don’t count every gram but I do track my big carb meals. Found out my body hates white bread but is chill with sourdough. Weird, right? Anyway, this guide is gold. I’m printing it out.
Patrick Marsh
December 1, 2025 AT 16:24Don’t forget: sugar alcohols vary. Erythritol? Almost zero impact. Maltitol? Not so much. Always check the type. And restaurant portions? Double what they say. Always.
Danny Nicholls
December 3, 2025 AT 08:44Just started carb counting last week and already my post-meal spikes are down. I used to think I was doing fine until I saw my CGM graph. Now I’m like a nerd with my food scale and emoji 🍞📉💊. Also-yes, you can have ice cream. Just don’t forget the insulin. I did. Twice. Lesson learned 😅