It’s easy to think of biotin as just another harmless vitamin-something you pop for shinier hair or stronger nails. But if you’re taking high-dose biotin supplements, you could be putting your life at risk-not from the supplement itself, but from what it does to your lab tests. The problem? Many common blood tests give false results when biotin is in your system. And those wrong numbers can lead to misdiagnoses, unnecessary surgeries, or even missed heart attacks.
How Biotin Messes With Your Blood Tests
Most automated lab tests use a technology called biotin-streptavidin binding. It’s a clever trick: biotin (a vitamin) sticks tightly to streptavidin (a protein), and scientists use that bond to grab and measure tiny amounts of hormones, enzymes, or proteins in your blood. It’s accurate, fast, and used in about 70% of all lab tests in the U.S. But when you take a high-dose biotin supplement-say, 5,000 to 10,000 micrograms a day-that extra biotin floods your bloodstream. Suddenly, there’s too much of it floating around. The lab’s test can’t tell the difference between the biotin it added and the biotin you took. So it gets confused. Results go haywire. The interference isn’t random. It depends on the type of test:- Sandwich immunoassays (like troponin, TSH, cortisol): Biotin causes falsely low results. This is dangerous because it can hide a heart attack or thyroid disease.
- Competitive immunoassays (like vitamin D, free T4, PTH): Biotin causes falsely high results. This can make you look like you have a condition you don’t have.
Tests Most at Risk-and Why It Matters
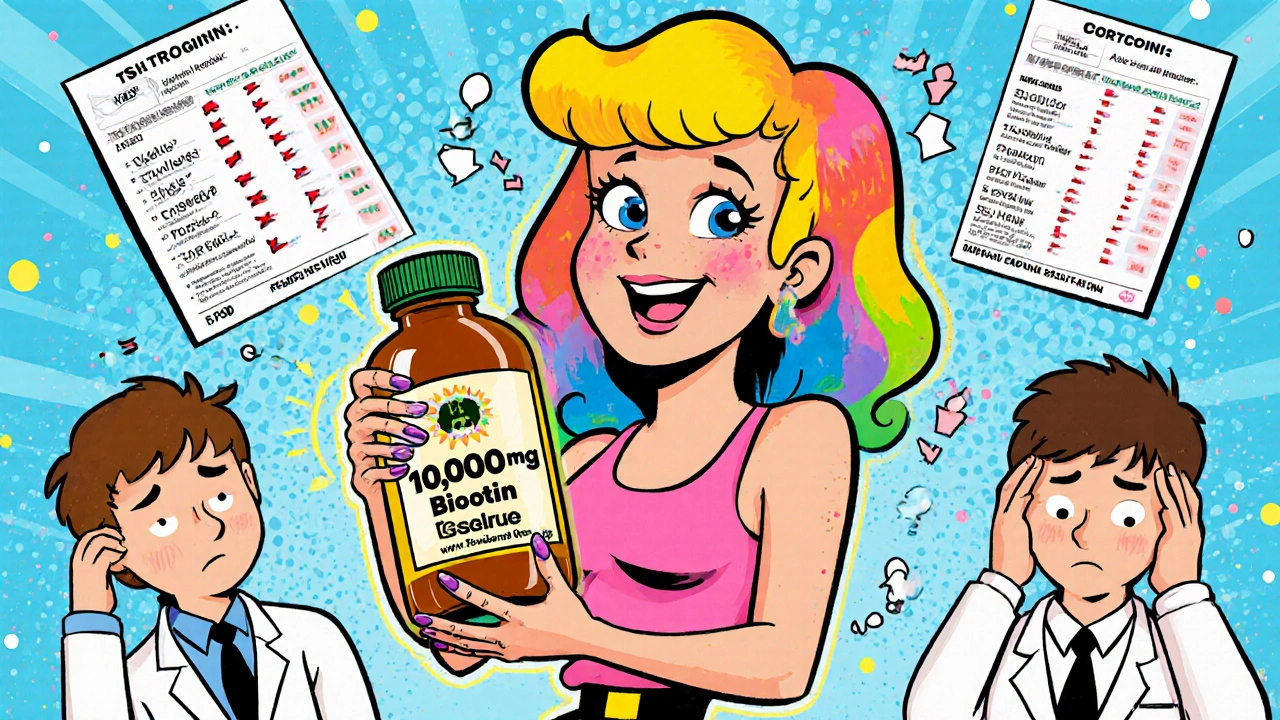
Some tests are more vulnerable than others. Here’s what can go wrong:- Troponin (heart attack test): Falsely low results mean doctors might miss a heart attack. In 2021, the FDA reported a death linked to this exact scenario-a patient with a heart attack was sent home because their troponin looked normal. They were taking 10,000 mcg of biotin daily for hair loss.
- Thyroid tests (TSH, fT4, fT3): Biotin can make your TSH look artificially low, mimicking hyperthyroidism. People have been treated with radioactive iodine or even had their thyroid removed because of this. One woman in a 2021 case study had a full thyroidectomy after her tests showed Graves’ disease-turns out, she was just taking a hair supplement.
- Cortisol and sex hormones: False highs or lows can lead to misdiagnosis of adrenal disorders or infertility. One patient was told she had low cortisol and put on steroid therapy for months, until her doctor asked about supplements.
- Vitamin D and parathyroid hormone: These can show up as abnormally high, making you look like you have a calcium disorder when you don’t.
And here’s the kicker: the lab report won’t say “biotin interference.” It just shows a number. If your doctor doesn’t know you’re taking biotin, they’ll treat the number-not you.
Who’s at Risk?
Not everyone who takes biotin is in danger. The problem starts at 5 milligrams (5,000 micrograms) per day. That’s 167 times the recommended daily intake of 30 mcg.- People taking hair, skin, and nail supplements: Many contain 5,000-10,000 mcg. These are sold as “beauty vitamins” and are often marketed as harmless. Most consumers don’t realize they’re taking a dose high enough to break lab tests.
- Multiple sclerosis patients: Some are prescribed up to 300 mg (300,000 mcg) daily under clinical protocols. That’s 10,000 times the daily requirement.
- Pregnant women on prenatal vitamins: Most prenatal vitamins have safe levels (30-100 mcg). But if you’re stacking them with a separate biotin pill, you could cross the danger line.
- People with biotinidase deficiency: They need high doses (5-10 mg) just to survive. Their labs are always tricky to interpret.
But here’s what most people don’t know: even if you think you’re being careful, you might be taking more than you realize. A 2022 study found that 89% of people taking biotin supplements didn’t tell their doctor. And 68% didn’t even know it could interfere with lab tests.
How Long Does Biotin Stay in Your System?
Biotin doesn’t vanish overnight. Its half-life is 8 to 24 hours, depending on the dose. That means:- After a single high-dose pill, it can take 24-48 hours for levels to drop enough to affect some tests.
- For thyroid and cardiac tests, labs recommend waiting 72 hours after your last dose.
- For people on 300 mg daily (MS patients), experts say to stop for 7 days before testing.
Some labs, like Quest Diagnostics, say 8 hours is enough. Others, like Labcorp and Vanderbilt, say 3 days. There’s no universal standard. That’s why you can’t rely on guesswork.
What You Should Do
If you’re taking biotin supplements, here’s what matters:- Know your dose. Check the label. If it says “5,000 mcg” or more, you’re in the danger zone.
- Stop taking it before any blood test. Don’t wait for your doctor to ask. Tell them you’re taking it-and ask how long to stop before testing.
- Don’t assume your doctor knows. In a 2020 survey, 43% of doctors didn’t know biotin could interfere with lab tests. You’re your own best advocate.
- Ask which tests you’re having. If it’s thyroid, cardiac, or hormone-related, biotin interference is a real concern.
- Don’t restart until after your results. Even if you feel fine, wait until your doctor confirms the results are accurate.
What Labs and Regulators Are Doing
The problem is getting attention. Since 2017, the FDA has issued multiple warnings. In 2021, they required supplement labels to include a warning if they contain over 100 mcg of biotin. Health Canada did the same. The College of American Pathologists says 89% of U.S. labs now screen for biotin interference. Newer lab machines are starting to fight back. Siemens launched “Biotin-Blocking Technology” in 2022, which cuts interference by 90%. But most machines still use the old system. And many supplements still don’t warn you. A 2022 analysis of 200 top-selling biotin products found that only 37% mentioned lab test interference on the label. That’s not just negligence-it’s a public health blind spot.
The Bigger Picture
The biotin supplement market is booming. It hit $358 million in 2022 and is expected to grow 7% yearly through 2030. Most of that growth comes from beauty products marketed to women under 40. The irony? Many of these women are also the ones getting regular blood tests-for thyroid issues, fertility, or general wellness. This isn’t a rare glitch. The FDA estimates that biotin interference affects 70 million lab tests per year in the U.S. That’s one in every 200 tests. And it’s preventable. The solution isn’t to stop taking biotin altogether. It’s to take it responsibly. If you’re taking 30-100 mcg from a multivitamin, you’re fine. But if you’re taking more, you need to treat it like a drug-not a cosmetic.What Happens When You Do It Right?
There are success stories. One patient in Vancouver had five years of misdiagnosed hyperthyroidism because of biotin. When her doctor finally asked about supplements, she stopped taking them. Her TSH returned to normal in two weeks. No radioactive treatment. No surgery. Just a simple conversation. Another patient in Ohio had a heart attack after being sent home with “normal” troponin levels. He was taking 10,000 mcg of biotin daily. After his case was reported, his hospital changed its protocol. Now, every patient gets asked about supplements before blood work. The fix isn’t complicated. It’s just not common enough.Can biotin supplements cause false positive or false negative lab results?
Yes. High-dose biotin (5,000 mcg or more per day) can cause both. In sandwich immunoassays-like troponin and TSH-it causes falsely low results, hiding conditions like heart attacks or hypothyroidism. In competitive immunoassays-like vitamin D and free T4-it causes falsely high results, making you appear to have a condition you don’t. The lab report won’t flag this; it just shows the wrong number.
How long should I stop taking biotin before a blood test?
It depends on your dose and the test. For most people taking 5,000-10,000 mcg daily, stop for at least 48-72 hours. For thyroid or cardiac tests, experts recommend 72 hours or longer. If you’re on high-dose therapy (like 300 mg daily for MS), stop for 7 days. Always check with your lab or doctor-guidelines vary. Never assume 8 hours is enough if you’re taking more than 5 mg.
Do all biotin supplements cause interference?
No. Only high doses do. The recommended daily intake is 30 mcg. Most multivitamins contain 30-300 mcg and are safe. The risk starts at 5,000 mcg (5 mg) per day. Hair, skin, and nail supplements often contain 5,000-10,000 mcg. Always check the label. If it says “10,000 mcg,” you’re in the danger zone.
Why don’t doctors always know about this?
Because it’s not taught in medical school. A 2020 study found that 43% of physicians didn’t know biotin could interfere with lab tests. Supplement labels rarely warn about it. And since the interference doesn’t show up on the report, doctors have no reason to suspect it. The burden is on you to speak up.
Are there any lab tests that aren’t affected by biotin?
Yes. Tests that don’t use biotin-streptavidin technology aren’t affected. These include mass spectrometry-based tests (like some hormone panels), certain point-of-care tests, and some newer platforms with biotin-blocking tech. But most routine tests-thyroid, cardiac, vitamin D, cortisol-are still vulnerable. Unless your lab tells you otherwise, assume the test is at risk.

Angela Gutschwager
November 19, 2025 AT 19:45This is wild-I took 10,000 mcg for my hair and didn’t even think twice. 😳
Andrew Montandon
November 20, 2025 AT 09:30Wow. I had no idea biotin could mess with troponin levels. I’ve been taking 5,000 mcg for months because my nail tech said it’d stop my ridges. Now I’m scared to get my annual bloodwork. I’ll stop it tomorrow. Thanks for the heads-up-this could’ve killed me. 😅
Andy Feltus
November 21, 2025 AT 01:23So let me get this straight… we’ve turned vitamins into a high-stakes game of medical Russian roulette, and the only rule is ‘trust your doctor’? Except your doctor probably doesn’t know about it either. Brilliant. 🙃
Dion Hetemi
November 22, 2025 AT 10:56Let’s be real-this isn’t a ‘public health blind spot.’ It’s a $358 million scam targeting women who think beauty is a biological function you can hack with pills. The supplement industry doesn’t care if you get misdiagnosed-they care if you keep buying. Wake up.
And don’t tell me ‘it’s just biotin.’ If it was harmless, why do they hide it in 20-point font under ‘other ingredients’? Why don’t they put ‘WARNING: MAY CAUSE DEATH BY MISDIAGNOSIS’ on the label? Because they’re profiting off your ignorance.
And now the FDA’s ‘solution’? A label warning at 100 mcg? That’s like saying ‘don’t drink bleach’ but letting them sell it in soda bottles labeled ‘energy boost.’
It’s not a glitch. It’s corporate negligence dressed up as ‘wellness.’
Kara Binning
November 24, 2025 AT 00:36I can’t believe this isn’t front-page news. I’m a woman in my 30s. I take biotin. I get thyroid tests. I’m lucky I didn’t get my thyroid ripped out because some company thought ‘glow’ was a medical claim. This is a gendered health crisis. They sell this to us like it’s makeup, then we pay with our bodies. I’m furious.
My mom had a thyroidectomy because of this. She’s been on levothyroxine ever since. She didn’t even know she was taking biotin-it was in her ‘hair, skin, nails’ pill. Now she’s got a scar and a lifelong hormone dependency because someone thought ‘beauty’ was more important than safety.
Why isn’t this a class-action lawsuit? Why isn’t the FTC shutting these brands down? We’re being treated like lab rats with credit cards.
Michael Petesch
November 24, 2025 AT 05:12As someone who works in clinical diagnostics, I can confirm: biotin interference is one of the most underreported and dangerous issues in lab medicine. We’ve had cases where patients were discharged with ‘normal’ troponin levels-only to return hours later in cardiac arrest. The lab report showed nothing wrong. The doctor trusted the number. The patient died.
Our lab now has a mandatory supplement questionnaire before any blood draw. We’ve also added a biotin flag to all thyroid and cardiac panels. But most clinics? Still flying blind.
And yes-this affects people globally. I’ve seen cases from India, Nigeria, Brazil. It’s not an American problem. It’s a systemic failure of regulation, education, and corporate ethics.
If you’re taking more than 300 mcg daily, assume every blood test is compromised until proven otherwise. And tell your doctor. Even if they roll their eyes.
Richard Risemberg
November 26, 2025 AT 01:18Imagine if your car’s speedometer could be fooled by a glitter sticker. You’d think you’re going 40 mph-until you crash into a tree. That’s biotin. It’s not a vitamin. It’s a lab test saboteur.
And yet, we’re told to ‘just be careful.’ No. We’re told to ‘take this for shinier hair’ and then left to die quietly because no one wants to admit that the wellness industry is built on lies.
I stopped taking mine. My hair didn’t fall out. My nails didn’t turn to dust. My bloodwork? Now it makes sense. I didn’t need the supplement. I needed a brain.
Reema Al-Zaheri
November 26, 2025 AT 09:41This is extremely concerning. I have been taking 5,000 mcg daily for two years for hair growth. I recently had a thyroid panel done, and my TSH was 0.18-I was told I had hyperthyroidism. I’m now terrified that this was all biotin interference. I will stop immediately and retest in 72 hours. Thank you for this detailed post-it could save lives.
Michael Salmon
November 28, 2025 AT 05:06Stop crying about biotin. If you’re dumb enough to take 10,000 mcg of a vitamin, you deserve whatever false result you get. This isn’t a medical crisis-it’s a ‘I didn’t read the label’ crisis. Also, your hair doesn’t need a vitamin bomb. It needs a haircut and a shower.
And yes, I know you think I’m harsh. Good. Maybe someone will finally stop buying this garbage.
Joe Durham
November 29, 2025 AT 01:23I used to take biotin because everyone on Instagram said it fixed their hair. Then I got my thyroid levels checked and they were all over the place. My doctor asked if I was taking supplements-I said yes, but didn’t think it mattered. He looked at me like I’d just admitted to drinking bleach.
I stopped. Two weeks later, my TSH went from 0.07 to 1.9. Normal. No meds. No surgery. Just… stopped taking the pill.
So yeah. Don’t be like me. Ask questions. Even if they feel silly.
Derron Vanderpoel
November 29, 2025 AT 11:09OMG I JUST REALIZED I’VE BEEN TAKING THIS FOR A YEAR 😭 I THOUGHT IT WAS JUST FOR HAIR AND NAILS… I GOT MY TSH DONE LAST MONTH AND THEY SAID I WAS HYPER… I’M SO SCARED NOW… I’LL STOP TOMORROW… PLEASE TELL ME I DIDN’T RUIN MY LIFE
Timothy Reed
November 30, 2025 AT 03:11Thank you for this comprehensive and urgently needed overview. As a primary care provider, I’ve encountered multiple cases of biotin-induced misdiagnosis over the past three years. The most troubling aspect is not the scientific mechanism-it’s the lack of patient awareness and provider education. We must integrate supplement screening into routine clinical workflows. I now include a standardized supplement checklist in all new patient intake forms. If you’re taking any over-the-counter product labeled ‘beauty,’ ‘hair,’ or ‘energy,’ disclose it. Even if you think it’s ‘just a vitamin.’
harenee hanapi
December 1, 2025 AT 03:15Everyone’s acting like this is news. I’ve been warning people for years. My sister took 10,000 mcg and got her thyroid removed. Now she’s on meds for life. And guess what? The supplement company didn’t even get fined. They just rebranded it as ‘glow boost.’ This system is broken. And no one’s paying attention until someone dies.
It’s always the women. Always.
Christopher Robinson
December 1, 2025 AT 20:51Just stopped my 5,000 mcg biotin today 🙌 I had no idea. My lab results were always weird but I thought I was just ‘anomalous.’ Now I feel like a genius for listening to this post. Also, I’m getting my troponin redone in 72 hours. Fingers crossed. 🤞
Andrew Montandon
December 2, 2025 AT 21:35Thanks for the replies, everyone. I just called my doctor and she said she’d never heard of this either. She’s going to reschedule my bloodwork for next week. I’m going to print out this article and hand it to her. Honestly? I think this needs to be mandatory info on every supplement bottle. Like cigarette warnings. ‘This may cause your doctor to miss a heart attack.’