What Are Arrhythmias?
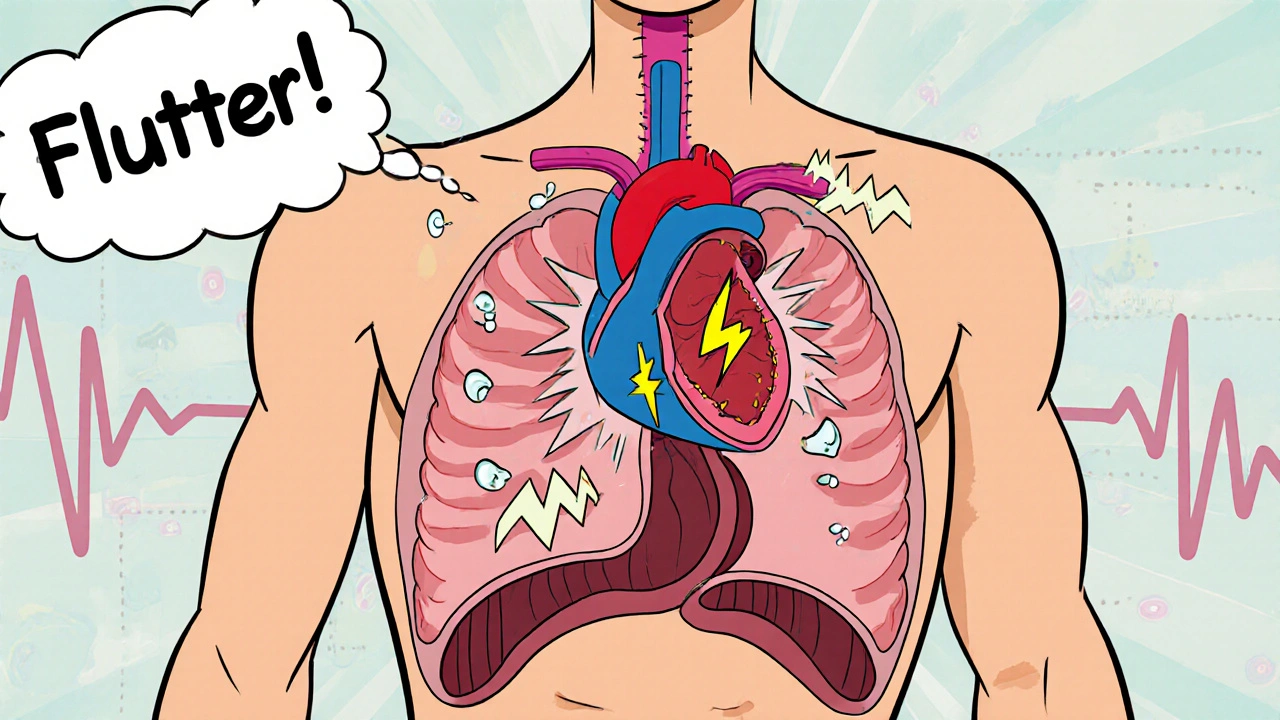
When your heart beats too fast, too slow, or irregularly, it’s not just a flutter-it’s an arrhythmia. Your heart relies on precise electrical signals to pump blood efficiently. When those signals go off track, your heart doesn’t work the way it should. Arrhythmias can feel like a skipped beat, a racing heart, or a slow, heavy thud in your chest. For some, they’re harmless. For others, they’re a warning sign of something serious.
Three of the most common types are atrial fibrillation, bradycardia, and tachycardia. Each has different causes, symptoms, and treatments. Knowing the difference matters-not just for diagnosis, but for knowing when to act.
Atrial Fibrillation: When the Upper Chambers Chaotic
Atrial fibrillation, or AFib, is the most common serious heart rhythm disorder. Instead of beating in a steady rhythm, the heart’s upper chambers (atria) quiver or fibrillate. This means blood doesn’t move properly, which can lead to clots-and clots can cause strokes.
The American Heart Association estimates 2.7 to 6.1 million Americans live with AFib. The risk goes up sharply after age 65. Many people don’t even know they have it until they have a stroke or their doctor notices an irregular pulse during a checkup.
Symptoms vary. Some feel:
- A fluttering or pounding in the chest
- Shortness of breath, especially during light activity
- Fatigue that won’t go away
- Dizziness or lightheadedness
- Chest discomfort
Others feel nothing at all. That’s why checking your pulse regularly matters. If it feels uneven or skips beats, don’t ignore it.
AFib isn’t one condition-it comes in stages. Paroxysmal AFib comes and goes on its own. Persistent AFib lasts longer than a week and needs treatment to reset. Permanent AFib means the heart can’t return to normal rhythm, so the focus shifts to controlling the rate and preventing clots.
How Is AFib Diagnosed?
There’s no single test you can do at home. Diagnosis starts with your doctor checking your pulse. If it’s irregular, the next step is almost always an electrocardiogram (ECG). This simple, painless test records your heart’s electrical activity and can spot AFib instantly.
But AFib doesn’t always show up during a short office visit. If symptoms come and go, your doctor might ask you to wear a portable monitor for 24 hours or longer. These devices-called Holter monitors or event recorders-capture your heart rhythm during daily life.
Other tests help figure out what’s causing the problem:
- Echocardiogram: Uses sound waves to check heart structure and valve function
- Blood tests: Look for thyroid issues, electrolyte imbalances, or kidney problems
- Chest X-ray: Checks for enlarged heart or lung conditions
- Stress test: Watches how your heart reacts to physical activity
It’s not just about finding AFib-it’s about finding why it’s happening. High blood pressure, sleep apnea, obesity, and heavy alcohol use are common triggers.
Treatment for Atrial Fibrillation
There’s no one-size-fits-all plan. Treatment depends on your symptoms, how long you’ve had AFib, and whether you have other health problems.
The two main goals are:
- Control your heart rate or rhythm
- Prevent blood clots and stroke
Most people start with medications. Rate-control drugs like beta-blockers or calcium channel blockers slow the heart down. Rhythm-control drugs like flecainide or amiodarone try to restore normal rhythm-but they come with side effects and aren’t always effective.
If medications don’t work, or if you’re young and otherwise healthy, your doctor might suggest a procedure called cardiac ablation. This uses heat or cold to create tiny scars in the heart tissue, blocking the faulty signals that cause AFib.
A newer technique called pulsed field ablation (PFA) uses electrical pulses instead of heat or cold. It’s faster, safer, and less likely to damage nearby tissues. It’s becoming more common in specialized centers.
For people with permanent AFib, a different option is AV node ablation combined with a pacemaker. This stops the irregular signals from reaching the lower chambers and lets the pacemaker take over.
But medication and procedures aren’t enough. Lifestyle changes are critical. Losing weight, cutting back on alcohol, managing blood pressure, and treating sleep apnea can reduce AFib episodes-even reverse them in some cases.
Bradycardia: When the Heart Beats Too Slow
Bradycardia means your heart beats fewer than 60 times per minute. Sounds bad? Not always. Athletes and very fit people often have slow heart rates-it’s a sign of a strong, efficient heart.
But if your heart beats too slowly and doesn’t pump enough blood, you’ll feel it. Symptoms include:
- Fainting or near-fainting
- Dizziness or lightheadedness
- Easy fatigue
- Shortness of breath
- Chest pain
- Confusion or trouble concentrating
Causes vary. It can be from aging, heart disease, heart attacks, or certain medications like beta-blockers. It can also be caused by an underactive thyroid or electrolyte imbalances.
In some cases, the heart’s natural pacemaker-the sinoatrial (SA) node-doesn’t fire properly. Or signals from the upper chambers don’t reach the lower chambers. This is called heart block.
Diagnosis is straightforward: an ECG will show the slow rhythm. A Holter monitor might be needed if it comes and goes.
Treatment depends on the cause. If a medication is to blame, your doctor might adjust the dose. If the problem is structural, a pacemaker is often the solution. Modern pacemakers are tiny, implanted under the skin, and can last 5 to 15 years. They’re life-changing for people whose hearts can’t keep up.
Tachycardia: When the Heart Races
Tachycardia means your heart beats more than 100 times per minute at rest. Like bradycardia, it’s not always dangerous. Exercise, stress, or caffeine can cause a temporary spike. But if your heart races without reason, it’s a problem.
There are several types:
- Supraventricular tachycardia (SVT): Starts in the upper chambers. Often sudden, with heart rates of 150-250 bpm. Feels like your heart is fluttering or pounding.
- Ventricular tachycardia (VT): Starts in the lower chambers. More dangerous. Can lead to cardiac arrest if not treated.
- Heart failure-related tachycardia: The heart speeds up to compensate for poor pumping.
Symptoms include palpitations, chest pain, dizziness, fainting, and shortness of breath. In severe cases, especially with VT, you can collapse without warning.
Diagnosis starts with an ECG. If it’s not happening during the test, you’ll need a monitor. Blood tests check for thyroid problems or electrolyte issues. An echocardiogram looks for structural damage.
Treatment varies. For SVT, simple tricks like the Valsalva maneuver (holding your breath and bearing down) can stop the episode. Medications like adenosine or beta-blockers are used for recurring cases. For VT, especially if you’ve had a heart attack, an implantable cardioverter-defibrillator (ICD) might be needed. It can shock your heart back to normal if it goes into a dangerous rhythm.
Some people benefit from ablation-just like with AFib. This is especially true for SVT, where a single abnormal pathway can be targeted and destroyed.
When to Worry
Not every skipped beat or fast heart rate is an emergency. But some signs mean you need help right away:
- Chest pain that lasts more than a few minutes
- Severe shortness of breath
- Fainting or near-fainting
- Heart rate over 150 bpm that doesn’t go away
- Confusion or slurred speech
If you have any of these, call for emergency help. Atrial fibrillation can lead to stroke. Ventricular tachycardia can lead to sudden death. Bradycardia can cause organ damage from poor blood flow.
Even if symptoms are mild, don’t wait. Many people ignore early signs until something serious happens. Regular checkups, knowing your pulse, and tracking symptoms can catch problems before they become crises.
Lifestyle That Protects Your Heart
No matter what type of arrhythmia you have-or might develop-your daily habits make a huge difference.
Here’s what works:
- Control blood pressure: High pressure strains the heart and increases AFib risk
- Lose excess weight: Even a 10% reduction can cut AFib episodes in half
- Limit alcohol: One drink a day can trigger AFib in some people
- Quit smoking: Smoking damages heart tissue and increases arrhythmia risk
- Treat sleep apnea: If you snore loudly or wake up gasping, get tested
- Manage stress: Chronic stress raises adrenaline and can trigger arrhythmias
- Exercise regularly: But don’t overdo it-extreme endurance sports can increase AFib risk in some
These aren’t just suggestions. They’re proven ways to reduce your risk and improve outcomes-even if you’ve already been diagnosed.
What Comes Next?
Arrhythmias are manageable. They’re not always curable, but they’re rarely a death sentence. With the right diagnosis, treatment, and lifestyle changes, most people live full, active lives.
If you’ve been told you have AFib, bradycardia, or tachycardia, don’t panic. Ask questions. Understand your options. Work with your doctor to build a plan that fits your life.
And if you haven’t been diagnosed-but you’ve felt your heart acting strange-don’t brush it off. Your pulse is a window into your heart’s health. Pay attention to it. It might just save your life.

Shannon Amos
November 27, 2025 AT 11:17Wendy Edwards
November 29, 2025 AT 05:18Jaspreet Kaur
November 29, 2025 AT 08:32Gina Banh
November 30, 2025 AT 13:22Deirdre Wilson
December 1, 2025 AT 11:54Damon Stangherlin
December 2, 2025 AT 20:30Ryan C
December 3, 2025 AT 23:39Dan Rua
December 4, 2025 AT 04:08Mqondisi Gumede
December 5, 2025 AT 00:13Douglas Fisher
December 5, 2025 AT 09:54Albert Guasch
December 7, 2025 AT 07:23Ginger Henderson
December 8, 2025 AT 07:02Bethany Buckley
December 8, 2025 AT 11:19Stephanie Deschenes
December 8, 2025 AT 22:42