For decades, women have been told to use backup birth control when taking antibiotics. It’s a warning passed down from friends, pharmacists, and even some doctors. But here’s the truth: most antibiotics don’t affect birth control pills. The fear isn’t based on science-it’s based on a myth that won’t die.
The Origin of the Myth
The idea that antibiotics ruin birth control started in the 1970s. Back then, a few women on the pill got pregnant while taking antibiotics. The obvious assumption? The antibiotics caused it. But those early reports were messy. They didn’t control for other factors-like missed pills, vomiting, or using the wrong type of antibiotic. The real culprit? One specific drug: rifampin. Rifampin, used to treat tuberculosis, was the only antibiotic shown to interfere with hormonal birth control. But because it had a similar-sounding name to other antibiotics like amoxicillin, the confusion stuck. Over time, the warning spread like gossip. And now, even though we have decades of solid research, many people still believe every antibiotic puts their birth control at risk.The Science: Only Two Antibiotics Really Matter
Let’s cut through the noise. Out of hundreds of antibiotics, only two have proven, significant interactions with birth control pills:- Rifampin (brand name Rifadin)
- Rifabutin (brand name Mycobutin)
Common Antibiotics That Are Safe
If you’ve been prescribed any of these, you don’t need to worry about your birth control:- Amoxicillin
- Azithromycin (Zithromax)
- Doxycycline
- Clarithromycin (Biaxin)
- Erythromycin
- Metronidazole (Flagyl)
- Ciprofloxacin (Cipro)
- Nitrofurantoin
- Amoxicillin-clavulanate (Augmentin)
What About Gut Bacteria?
One popular theory says antibiotics kill gut bacteria that help recycle estrogen. Less recycling = less hormone available = birth control fails. It sounds logical. But it doesn’t hold up. The amount of estrogen that gets recycled through the gut is tiny. Even if antibiotics wiped out half your gut flora-which they don’t-the body still gets plenty of hormone from the pill itself. A 2011 study in the journal Contraception measured estrogen levels in women taking amoxicillin. Results? No change. Serum estradiol stayed between 200-400 pg/mL-the same as when they weren’t on antibiotics. Your gut isn’t the gatekeeper of your birth control. Your liver is. And only rifampin and griseofulvin trigger the liver to break down hormones faster.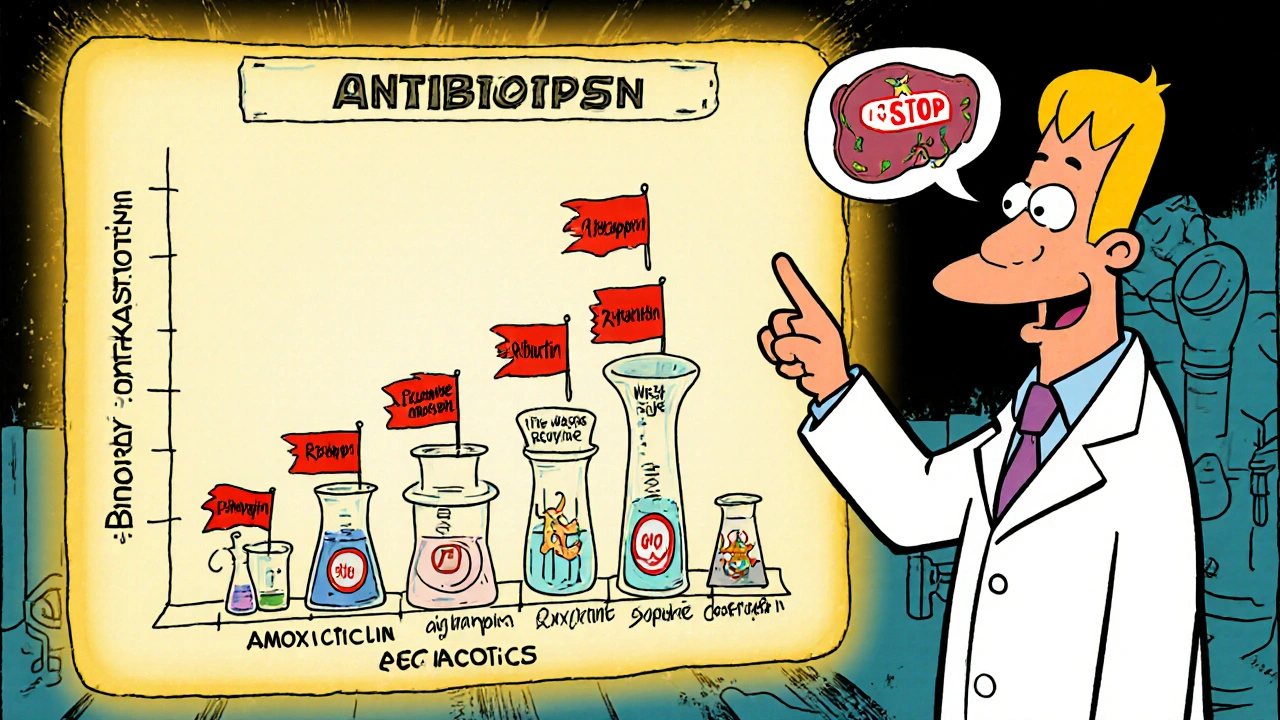
Other Drugs That Actually Do Interfere
If you’re worried about birth control effectiveness, don’t just focus on antibiotics. Some other common medications are far more likely to cause problems:- Lamotrigine (for seizures)-at doses over 300 mg/day
- Topiramate (for seizures or migraines)-at doses over 200 mg/day
- Efavirenz and nevirapine (HIV medications)
- St. John’s wort (herbal supplement)-reduces estrogen by up to 57%
Why Do Pharmacists Still Warn People?
You’ve probably heard it: “Just to be safe, use condoms.” But why do so many pharmacists still say this-even though the science says it’s unnecessary? A 2022 study in the Journal of the American Pharmacists Association found that 35% of pharmacists still recommend backup contraception for all antibiotics. Why? Fear. Liability. Tradition. It’s easier to say “use a condom” than to explain the difference between rifampin and amoxicillin. It’s safer for the pharmacy to avoid a lawsuit than to risk being wrong-even if the risk is near zero. And many providers just never updated their knowledge after the 2016 CDC guidelines. But here’s the problem: unnecessary warnings cause real harm. Women stop taking their pills because they think they’re not working. Others feel anxious and confused. Some even switch to less effective methods like condoms alone, increasing their actual risk of pregnancy.What Should You Do?
Here’s the simple, science-backed guide:- If your antibiotic is rifampin or rifabutin: Use backup contraception (condoms, diaphragm, or copper IUD) for 28 days after finishing the course. This applies to all hormonal birth control: pills, patches, rings.
- If your antibiotic is griseofulvin: Same rule-backup for 28 days.
- If your antibiotic is anything else: No backup needed. Your birth control works just fine.
What About the Cases of Pregnancy?
You’ve probably heard stories: “I got pregnant while on amoxicillin.” Or “I took doxycycline and missed my period.” In almost every case, the real issue wasn’t the antibiotic. It was:- Missed pills
- Vomiting or diarrhea within two hours of taking the pill
- Starting a new pack late
- Taking rifampin without knowing it
What’s Changing Now?
In January 2023, the FDA updated the labeling on all hormonal contraceptives. For the first time, they explicitly state:“Rifampin, rifabutin, and griseofulvin may reduce effectiveness. Other antibiotics do not affect effectiveness.”That’s huge. It’s official. No more ambiguity. Major medical groups are also pushing back. The American College of Obstetricians and Gynecologists (ACOG) says backup contraception isn’t needed for non-rifamycin antibiotics. The CDC says the same. Dr. Jen Gunter, a well-known OB/GYN and author, calls the myth “a dangerous piece of medical folklore.”
Final Advice: Talk to Your Doctor
You don’t have to guess. If you’re on birth control and prescribed an antibiotic, ask:- “Is this rifampin or rifabutin?”
- “Does this interact with my birth control?”
- “Do I need backup?”
Do all antibiotics reduce the effectiveness of birth control pills?
No. Only two antibiotics-rifampin and rifabutin-have been proven to reduce hormone levels enough to affect birth control. Griseofulvin, an antifungal, also has this effect. All other common antibiotics, including amoxicillin, azithromycin, doxycycline, and metronidazole, do not interfere with birth control pills according to the CDC and ACOG.
What should I do if I’m prescribed rifampin while on birth control?
Use a backup method of contraception, like condoms or a diaphragm, for 28 days after finishing your rifampin course. This applies to all forms of hormonal birth control, including pills, patches, and vaginal rings. Do not rely on your birth control alone during this time.
Can I get pregnant while taking amoxicillin and birth control?
No, not because of the amoxicillin. Amoxicillin does not affect the hormones in birth control pills. If pregnancy occurs while taking both, the cause is likely missed pills, vomiting, or other user-related factors-not the antibiotic.
Why do some pharmacists still say to use backup contraception with antibiotics?
Many pharmacists continue this advice out of caution, fear of liability, or because they haven’t updated their knowledge since older guidelines. A 2022 study found 35% of pharmacists still recommend backup contraception for all antibiotics, despite clear evidence that only rifampin and rifabutin require it. This practice can cause unnecessary anxiety and lead to poor contraceptive choices.
Does St. John’s wort affect birth control?
Yes. St. John’s wort, a popular herbal supplement for mood, can reduce estrogen levels by up to 57%. This significantly lowers birth control effectiveness. If you’re taking it, you should use a backup method or switch to a non-hormonal form of contraception.
What about rifaximin? Is it the same as rifampin?
No. Rifaximin (brand name Xifaxan) is a different drug used for traveler’s diarrhea and gut infections. Unlike rifampin, it doesn’t get absorbed into the bloodstream and doesn’t affect liver enzymes. It has no interaction with birth control pills and does not require backup contraception.
Should I stop taking my birth control if I’m on antibiotics?
Never stop taking your birth control unless your doctor tells you to. Stopping increases your risk of pregnancy more than any antibiotic (except rifampin or rifabutin). If you’re unsure about your specific medication, check the name and ask your provider-don’t guess.


Richard Wöhrl
November 22, 2025 AT 16:03Okay, I’ve been waiting for someone to finally debunk this myth properly. I’m a pharmacist, and I’ve seen this confusion daily-patients panicking because they got amoxicillin and suddenly think their birth control is useless. The science is clear: only rifampin and rifabutin matter. Griseofulvin? Yeah, that’s a sneaky one, but it’s rare. The rest? Zero impact. It’s not just outdated advice-it’s harmful. Women stop taking their pills because they’re scared, and then they get pregnant. That’s not safety. That’s fearmongering dressed up as caution.
And don’t even get me started on pharmacists who just say ‘use condoms’ without checking the drug. It’s lazy. We’re trained to assess interactions, not just recite old pamphlets. The FDA updated their labeling in 2023. This isn’t 1998 anymore.