When your body doesn’t get enough iron, vitamin B12, or folate, it doesn’t just make you tired. It can also make your allergies worse. Many people with food allergies notice their symptoms flare up more often or more severely when they’re low on key nutrients. It’s not coincidence. There’s a real, measurable link between anemia caused by nutritional deficiencies and how your immune system reacts to allergens.
What happens when you’re low on iron?
Iron isn’t just for making red blood cells. It’s also critical for immune function. When iron levels drop, your body can’t produce enough T-regulatory cells - the immune system’s peacekeepers. These cells normally keep allergic responses in check. Without them, your body overreacts to harmless proteins in foods like peanuts, milk, or eggs.
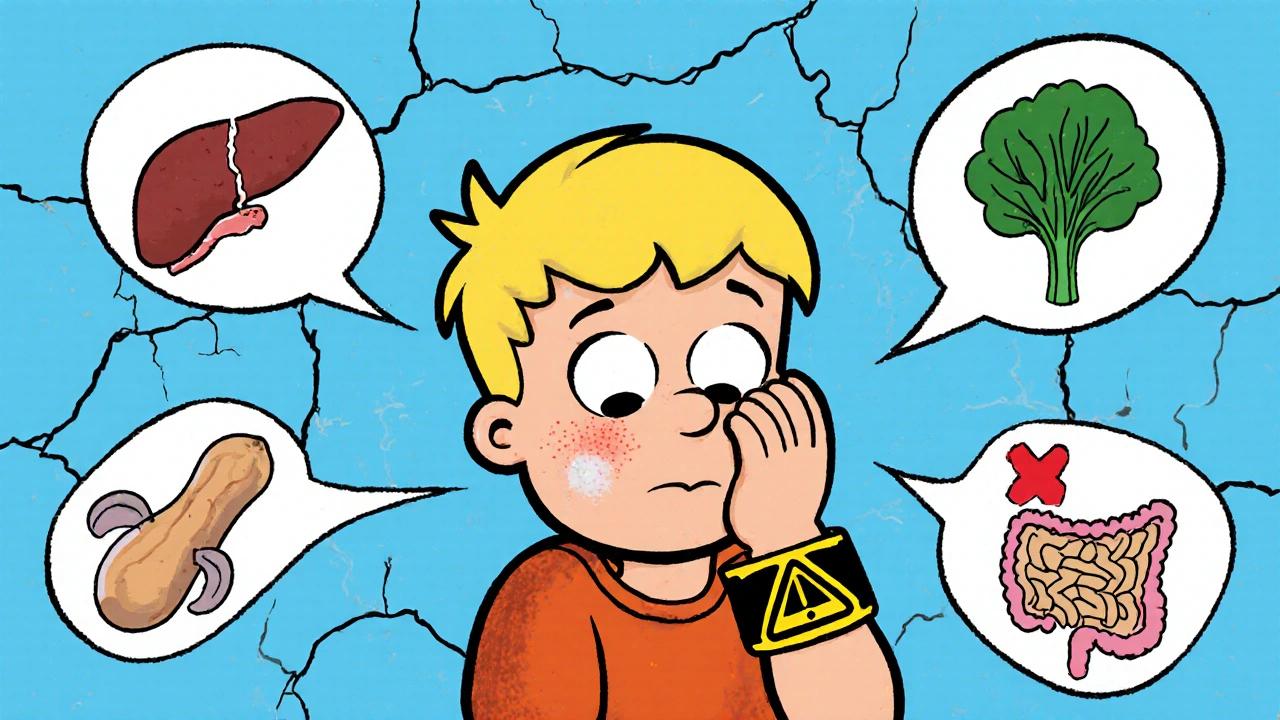
Studies show that children with iron deficiency anemia are nearly twice as likely to develop food allergies compared to those with normal iron levels. In adults, low ferritin (the stored form of iron) correlates with higher levels of IgE antibodies - the immune markers that trigger hives, swelling, and anaphylaxis. One 2023 study tracking 1,200 adults with peanut allergies found that those with ferritin below 30 ng/mL had 3.5 times more severe reactions than those with ferritin above 50 ng/mL.
It’s not just about how much iron you eat. It’s about how well you absorb it. People with celiac disease or eosinophilic esophagitis - both linked to food allergies - often have damaged intestines that block iron uptake. That creates a vicious cycle: allergy → gut damage → iron deficiency → worse allergies.
Vitamin B12 and folate: The silent players
Iron isn’t the only nutrient that matters. Vitamin B12 and folate are equally important for immune balance. These vitamins help your body make and repair DNA. When they’re low, your immune cells don’t mature properly. That leads to a skewed immune response - more Th2 activity (the allergic pathway) and less Th1 (the infection-fighting pathway).
People with pernicious anemia, a condition where the body can’t absorb B12, often report worsening eczema, asthma, and food-induced nausea. Folate deficiency, common in people who avoid leafy greens or take certain medications like methotrexate, has been tied to higher rates of shellfish and soy allergies in clinical trials.
One overlooked fact: many plant-based diets are low in B12. Vegans and vegetarians with food allergies may be at double risk - they’re avoiding allergens like dairy or eggs, but also missing key nutrients found in those same foods. Without careful planning, their immune system becomes more reactive, not less.
The gut connection: Where nutrition and allergies meet
Your gut is where food allergies and nutritional deficiencies collide. A leaky gut - caused by chronic inflammation from food allergens - lets undigested proteins slip into your bloodstream. Your immune system sees them as invaders and mounts a response. But if you’re already low on iron or B12, your gut lining can’t heal properly.
Zinc, another nutrient often low in people with food allergies, helps repair the gut barrier. Magnesium supports immune cell signaling. Vitamin D regulates the tolerance of your immune system to food proteins. When all these nutrients are missing, your gut stays inflamed, your immune system stays confused, and your allergic reactions get worse.
It’s not uncommon for someone with multiple food allergies to also have low hemoglobin, low ferritin, and low vitamin D - all at the same time. Treating just the allergies with avoidance or epinephrine doesn’t fix the root cause. The body needs the building blocks to reset its immune balance.
What foods help - and what makes it worse
Not all iron-rich foods are created equal. Heme iron from meat, poultry, and fish is absorbed 3-5 times better than non-heme iron from spinach or lentils. If you’re allergic to dairy, you’re missing out on vitamin D and calcium, which both help iron absorption. If you avoid eggs, you lose choline and B12. If you’re allergic to nuts, you lose zinc and magnesium.
Here’s what works:
- Beef liver - one of the richest sources of iron, B12, and folate. A 3-ounce serving gives you 100% of your daily iron needs.
- Clams and oysters - packed with iron and zinc. One serving can provide 20 times your daily zinc requirement.
- Fortified nutritional yeast - a vegan-friendly source of B12 and folate. Look for brands that add 100% DV per tablespoon.
- Dark leafy greens with lemon juice - vitamin C boosts non-heme iron absorption. Spinach alone won’t cut it, but spinach + orange slices will.
And here’s what to avoid:
- Tea and coffee with meals - tannins block iron absorption.
- Calcium supplements taken with iron - they compete for the same absorption pathway.
- Processed foods labeled “allergen-free” - they’re often stripped of nutrients and loaded with sugar to mask flavor, which worsens inflammation.
Testing and fixing the gap
If you have food allergies and feel constantly tired, dizzy, or short of breath, get tested. Don’t just check hemoglobin. Ask for:
- Ferritin (target: 50-100 ng/mL)
- Serum B12 (target: 500-900 pg/mL)
- Folate (target: 15-20 ng/mL)
- Vitamin D (target: 40-60 ng/mL)
- Zinc (target: 80-120 mcg/dL)
Many doctors only test for hemoglobin. That’s like checking if your car has gas - but ignoring the oil, battery, and spark plugs. You might think you’re fine because you’re not anemic yet. But your immune system is already running on empty.
Supplements can help, but they’re not magic. Iron pills can cause nausea or constipation. B12 injections work better than pills if you have absorption issues. The best approach? Combine targeted nutrition with medical guidance.
Work with a dietitian who understands both food allergies and nutritional anemia. They can help you find safe, nutrient-dense alternatives. For example, if you’re allergic to shellfish, try grass-fed beef or pasture-raised chicken liver. If you’re allergic to eggs, try sunflower seeds and pumpkin seeds for zinc and magnesium.
Real results: What recovery looks like
One mother in Adelaide, Australia, noticed her 8-year-old son’s peanut allergy reactions got worse every winter. He was pale, tired, and had chronic eczema. Blood tests showed ferritin at 12 ng/mL and B12 at 200 pg/mL. After three months of iron supplements, weekly liver pâté (made with chicken liver), and daily vitamin D drops, his ferritin rose to 68 ng/mL. His reactions became milder - no more epinephrine use. His eczema cleared up. He started sleeping through the night.
Another patient, a 34-year-old vegan with dairy and soy allergies, had been avoiding all major allergens but still got hives weekly. Her diet was full of rice milk, gluten-free bread, and processed snacks. Her B12 was 180 pg/mL, iron 8 mg/L. After switching to fortified nutritional yeast, daily seaweed snacks, and weekly lentil stew with lemon, her symptoms dropped by 70% in six weeks.
These aren’t outliers. They’re predictable outcomes when you treat the body as a whole system - not just the allergy symptoms.
Bottom line: Nutrition isn’t optional
Food allergies aren’t just about avoiding triggers. They’re about giving your body the tools to stay calm. If you’re low on iron, B12, folate, zinc, or vitamin D, your immune system has no choice but to overreact. You can avoid peanuts all you want - but if your body lacks the nutrients to regulate itself, you’ll still get sick.
Fixing nutritional deficiencies doesn’t cure food allergies. But it can make them manageable. It can mean fewer emergency visits, less reliance on medication, and a life with more freedom - not just more restrictions.
Start with a blood test. Don’t wait until you’re exhausted. Don’t assume your diet is enough because you eat “healthy.” Many people with food allergies are secretly malnourished. Their bodies are starving - not from lack of food, but from lack of the right nutrients.
Can anemia cause food allergies?
No, anemia doesn’t cause food allergies. But it can make them worse. Low iron, B12, or folate weakens the immune system’s ability to tolerate food proteins, leading to more frequent or severe allergic reactions. It’s a multiplier effect, not a cause.
Should I take iron supplements if I have food allergies?
Only if your blood tests show low iron. Taking iron without knowing your levels can cause side effects like nausea, constipation, or even iron overload. Always get tested first. If you’re allergic to iron-rich foods like red meat, talk to a dietitian about safe alternatives like fortified cereals or plant-based iron with vitamin C.
Why do my allergy symptoms get worse in winter?
Winter brings less sunlight, which lowers vitamin D - a key regulator of immune tolerance. Many people also eat fewer fresh foods and rely on processed, allergen-free snacks that lack nutrients. Low vitamin D plus poor nutrition = more inflammation and worse reactions. Testing your vitamin D and iron levels in late fall can help you prepare.
Can a vegan diet increase the risk of food allergies?
Not directly. But a poorly planned vegan diet often lacks B12, iron, zinc, and omega-3s - nutrients that help calm immune responses. If you’re also avoiding common allergens like soy or gluten, you’re cutting out even more nutrient sources. The risk isn’t from being vegan - it’s from not replacing those nutrients with safe, nutrient-dense foods.
Is there a test to see if my allergies are linked to nutritional deficiencies?
Yes. Ask your doctor for a full nutritional panel: ferritin, serum B12, folate, vitamin D, zinc, and magnesium. Combine that with your allergy history and symptom patterns. If your IgE levels are high and your nutrient levels are low, there’s a strong connection. Treating the deficiency often reduces allergic symptoms - even without changing your avoidance diet.

Bruce Bain
November 19, 2025 AT 13:04So if you're allergic to eggs and dairy, and you're vegan, you're basically running on fumes? That makes sense. My cousin went from constant hives to zero symptoms after eating liver once a week. No joke.
deepak kumar
November 20, 2025 AT 20:52As someone from India where iron deficiency is common, I’ve seen this first-hand. Many kids with eczema and peanut allergies improve drastically after adding lentils + lemon juice + chicken liver to their diet. Nutrition isn’t magic-it’s medicine. 🙏
Dave Pritchard
November 21, 2025 AT 20:24This is such an important perspective. So many people think avoiding allergens is the whole game-but if your body doesn’t have the tools to heal, you’re just putting a bandage on a broken bone. Thank you for highlighting the real fix.
kim pu
November 22, 2025 AT 23:19Or maybe Big Pharma just doesn’t want you to know you can fix this with liver and sunlight instead of $500 epinephrine pens? 😏
Jonathan Gabriel
November 24, 2025 AT 02:56Wait-so you’re telling me the reason my kid’s peanut allergy went from ‘emergency room every winter’ to ‘mild sneeze’ after we started giving him chicken liver pâté is… because his immune system finally had iron? Not because the stars aligned? Not because the moon was in the seventh house? I feel like I’ve been sold a bill of goods by allergists who’ve never eaten a steak.
And why does no one talk about how ‘gluten-free’ crackers are just sugar bricks with a side of despair? I’m starting to think ‘allergen-free’ is just corporate speak for ‘nutrient void’.
Also-tea with meals? That’s not just a habit. That’s a slow-motion immune sabotage. Who wrote the rulebook on this? A Victorian tea lady with a grudge?
And why do we treat ferritin like it’s a secret club? If your hemoglobin’s fine, you’re ‘good’? Bro. Your immune cells are starving in the basement while you’re sipping oat milk lattes.
It’s not that we don’t know this stuff. It’s that the system doesn’t incentivize it. Doctors get paid for prescriptions, not for teaching people how to cook liver.
And yet-somehow-this post got more useful than 90% of medical journals I’ve read. That’s the real tragedy.
benedict nwokedi
November 25, 2025 AT 11:52They don’t want you to know this because if people fixed their allergies with food, the entire $40B allergy industry collapses. Big Pharma, Big Insurance, Big Allergist-everything’s built on keeping you dependent. The ‘test your ferritin’ advice? That’s a trap. They’ll sell you a $300 panel, then charge you $200 for the ‘consult’ to tell you to eat liver. Classic.
And why is nutritional advice always wrapped in ‘eat more liver’? Why not just inject us with synthetic immune regulators? Because it’s cheaper to let people suffer than to fund real research. This isn’t science-it’s a cover-up.
And don’t get me started on ‘fortified nutritional yeast.’ Who thought that was a good idea? It’s basically yeast with a government stamp. Next they’ll tell us to chew on chalk for calcium.
They’re gaslighting us. You think you’re eating ‘healthy’? You’re just a walking nutrient desert with a gluten-free label.
Duncan Prowel
November 27, 2025 AT 08:18While the correlation between nutritional deficiencies and exacerbated allergic responses is well-documented in peer-reviewed immunology literature, one must exercise caution in extrapolating causality from observational cohort studies. The 2023 study referenced, while statistically significant, does not control for confounding variables such as socioeconomic status, dietary diversity, or environmental allergen exposure. Moreover, the biological plausibility of iron-mediated T-regulatory modulation is supported by murine models, yet human translational evidence remains limited in scope. A more rigorous approach would involve randomized, double-blind, placebo-controlled trials assessing immune biomarker shifts following targeted micronutrient repletion. Until such evidence is established, clinical recommendations should remain provisional.
malik recoba
November 27, 2025 AT 09:10i had no idea this was even a thing… my kid’s eczema got better after we started giving him pumpkin seeds and orange slices. i thought it was just luck. thanks for putting this all together. i’m gonna get his blood checked this week. 🙏
Sarbjit Singh
November 28, 2025 AT 11:26Bro this is gold! 😍 I’m vegan and allergic to soy and nuts. Was feeling tired all the time. Started eating seaweed snacks and lentils with lemon. My skin cleared up in 3 weeks! 🙌 You’re right-nutrition is the real MVP. Thanks for sharing!
Sameer Tawde
November 29, 2025 AT 16:16Stop treating allergies like a puzzle you solve by removing pieces. Start treating them like a garden-you need the right soil, water, and sunlight. Iron, B12, zinc? That’s your fertilizer. Skip it, and even the best avoidance plan will fail.
Angela J
November 29, 2025 AT 17:18Wait… so they’re hiding this because if people ate liver, they wouldn’t need epinephrine auto-injectors? And the FDA knows? And they’re letting people die? This is a genocide. I’m not even kidding. My cousin’s son died because his doctor didn’t check ferritin. They let him die for profit.
Don Angel
December 1, 2025 AT 10:49Okay, I just want to say-this is the most useful thing I’ve read all year. I’ve been avoiding dairy and eggs for years. Thought I was eating clean. Turns out I was just eating white bread and rice cakes. No wonder I felt like a zombie. I’m getting my blood tested tomorrow. Thank you.
Erica Lundy
December 1, 2025 AT 18:25The epistemological framework underpinning this argument presumes a reductionist model of immunological function-one that privileges micronutrient status as the primary determinant of immune tolerance, thereby marginalizing the complex interplay of genetic predisposition, microbiome dynamics, and environmental epigenetics. While the clinical observations are compelling, they risk reinforcing a nutritional determinism that obscures the broader systemic nature of allergic pathogenesis. The body is not a machine to be calibrated with iron supplements; it is an emergent, adaptive system whose homeostasis cannot be reduced to the sum of its micronutrient parts.
That said, the practical utility of this approach for individuals suffering from intractable allergic symptoms remains undeniable. One must therefore navigate the tension between theoretical nuance and therapeutic pragmatism-an epistemic dilemma that mirrors the broader crisis in modern medicine.
Jonathan Gabriel
December 2, 2025 AT 07:16Erica, you just wrote a 12-sentence philosophy paper on liver. I love you. But let’s be real-your body doesn’t care if it’s ‘emergent’ or ‘adaptive’ when it’s covered in hives and you can’t sleep. It just wants the damn iron.
And if the FDA wants to keep selling EpiPens, fine. But I’m giving my kid pâté. Let them sue me for vitamin B12.